The NIHR physical activity evidence review will be an invaluable tool to anyone working in practice or policy. Evidence should be one of the key building blocks for any decisions. It helps decision makers determine what works and what doesn’t, what should be commissioned and prioritised, and (equally important) what should be stopped. The beauty of this review is that it brings together a range of evidence in a concise way, and comes with clear prompts to consider how to practically apply the findings.
Sarah Ruane, Strategic Lead for Health, Sport England
Executive summary
Being active matters because it is an important way of staying healthy. We know that people can reduce their risk of many serious diseases by staying physically active. Activity is also important for mental well-being and keeping socially connected. Finding enjoyable ways to be active can benefit people in so many ways. But it is often hard for people to start and keep the habit of regular activity. Around a quarter of people are inactive and less than two thirds meet recommended activity levels. We need to know more about what works in getting people active and sustaining this, particularly for those who are least active now. This review focuses on National Institute for Health Research (NIHR)-funded research evaluating interventions to increase physical activity for individuals and populations. This features over 50 published and ongoing studies. Evaluations range from programmes in schools and communities to changes in transport and the environment, which are designed to promote greater activity.
Early years and young children of primary school age
From the few studies available, it appears that there is no single best way to help parents, nursery schools and others to encourage and promote healthy activity during the early years. Small changes everywhere are probably required to help to keep young children active throughout the day. Much attention has focused on primary school aged children. Two large trials of healthy lifestyle programmes in schools showed little effect on activity but some positive changes in other areas like unhealthy snacking. A review of evaluations of changes to playgrounds to encourage a range of activities showed mixed results.
Young people of secondary school age
There are different challenges to get teenagers and young people active once they enter secondary school. Research based on what we know about behaviour change emphasises the importance of young people having some control over lifestyle choices. Two large trials focused on girls, who often are least active at this age, but interventions from dance to whole school programmes showed little effect. Other studies looked at wider changes to the environment. Free bus passes in London increased use of buses and did not displace walking or cycling. One area which retained free access to swimming pools saw more people swimming, particularly children, including those from most deprived areas. Studies suggest that a range of changes are needed both to encourage deliberate exercise and to build activity into the everyday routines of young people.
Introduction
About this review
This report brings together recent evidence on ways to influence physical activity behaviours in individuals and populations. This report focuses on studies funded by NIHR. Its purpose is to bring together NIHR-funded research, raising awareness of the findings and relating them to a broader body of research, but it is not a comprehensive review of all available evidence.
The NIHR was set up in 2006 to provide a comprehensive health research system focused on the needs of patients and the public. Since then it has funded a number of programmes, projects, and research centres related to physical activity and public health. These different studies have not been brought together in this way before.
We have looked through the portfolio of NIHR-funded research and identified studies with a focus on increasing physical activity in everyday life, and whose findings are most relevant for those who support the health and well-being of communities. These decision makers may work across a range of roles and organisations, in healthcare, local authorities, community organisations, education, or private companies. Prompts for reflection after each chapter are intended to encourage you to consider how the research may be helpful to you and your local communities. In order to retain our focus, we have had to exclude a wider body of evidence from the NIHR and other funders which focuses on the health benefits of physical activity. Such evidence is well represented in guidelines on physical activity from the UK Chief Medical Officers (updated guidelines are expected in autumn 2019), and NICE quality standards for physical activity. Studies have been selected with help from an expert group of relevant stakeholders listed in the acknowledgements section.
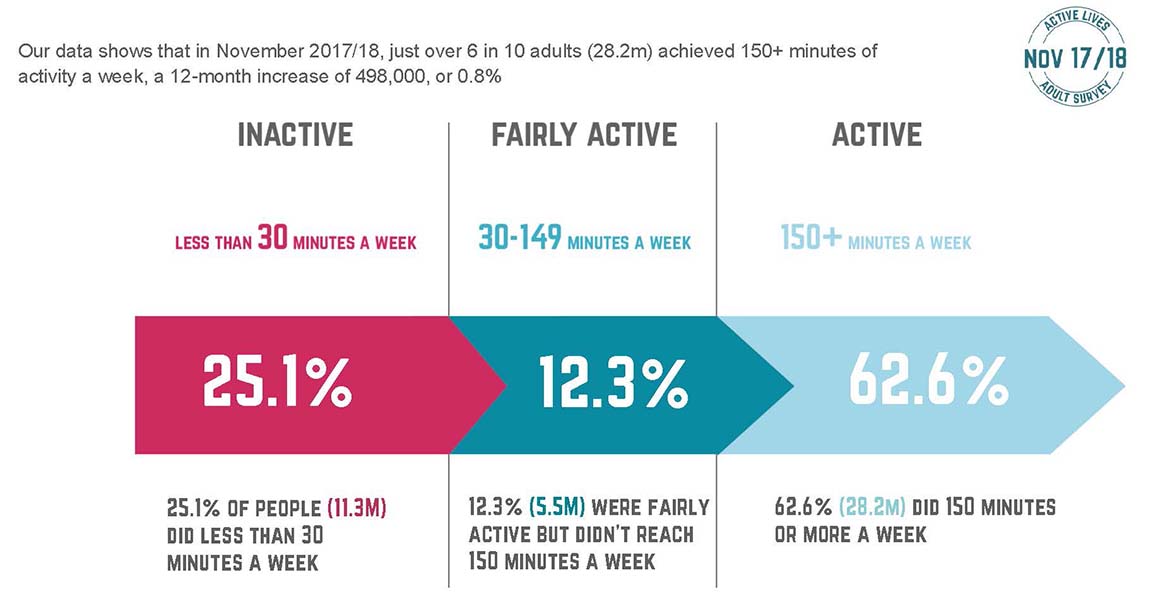
Figure 1: Physical activity levels of adults. Sport England Active Lives adult survey (xiv)
While many gaps in the evidence remain, we are pleased to share research that has identified useful components that can together help our communities to become more physically active. We hope this review will also help to identify areas for future research that will provide important understanding of how to increase physical activity for everyone.
Research included in this review
We have primarily included in this review NIHR-funded studies that assess ways to increase physical activity through individual, community, and environmental interventions. Studies that address physical activity as part of a larger suite of measures are included if they report changes in physical activity.
We have excluded many otherwise important studies that: did not involve interventions to try to change physical activity; that were exploratory or focused on research methods; that selected participants on the basis of their having defined clinical conditions; or that used exercise as therapy.
Although not included here, many funders other than the NIHR also support important work to develop the understanding of physical activity. Notable funders include the Medical Research Council, What Works Centres, the Big Lottery Fund, Sport England, and the Wellcome Trust.
Approach to physical activity
We have taken physical activity to mean any bodily movement produced by skeletal muscles that results in energy expenditure. Types of physical activity in daily life include occupational, transport, sports, conditioning, household, leisure, and other activities. This is broader than exercise, which refers to physical activity that is planned, structured, and repetitive and has as a final or an intermediate objective the improvement or maintenance of physical fitness (ii).
In considering physical activity, researchers often differentiate aerobic physical activity, strength and balance activity, and sedentary behaviour. All have important health effects, and guidelines usually recommend considering all three. Additionally, the ways in which people may be active or sedentary vary, as part of their leisure or work, through travel, and through sport or exercise.
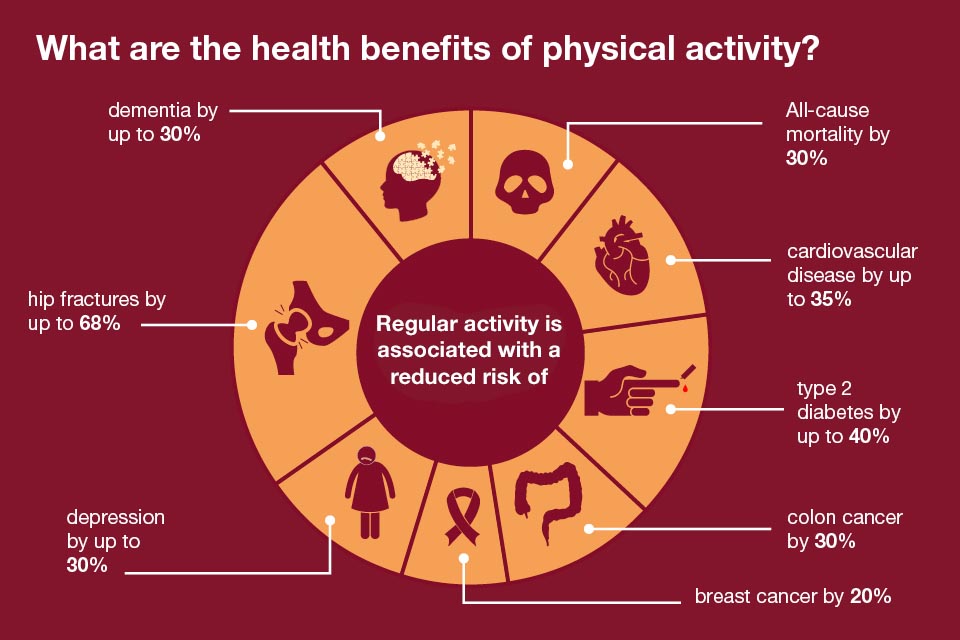
Figure 2: Health benefits of physical activity for adults.(i) Public Health England.
This review takes a life-course approach, considering the changing needs and opportunities of different age groups from infancy onwards, as well as considering interventions in the workplace and in the built and natural environments. This reflects the fact that people’s physical activity behaviours depend on the characteristics and attitudes of individuals, as well as the wider contexts and environments in which they live. In order to influence a person’s physical activity behaviours effectively, it will help to tailor any intervention in light of the whole system of factors that influence their behaviour, and the aspects that can be most effectively influenced.
Much research aggregates results for large numbers of people, and understanding the commonalities of what makes an intervention work is important to developing a science of behaviour. However, it is important to keep in mind the diversity of people and circumstances involved, to consider reasons why what works for one person may not work for another, and to adapt interventions to particular contexts. Understanding and addressing inequalities is essential in order to generate the greatest health and well-being benefits from physical activity. These inequalities often relate to social and cultural norms, economic factors, gender, geography, ethnicity, and a person’s current health. A finegrained understanding of the specific barriers that groups and individuals face is essential for effective interventions to be made available to those who may benefit most.
Move more, eat better, reduce alcohol, don’t smoke. Blah, drone, lecture… this isn’t nearly enough. We need to think not only about the things we can do for ourselves, but about how physical activity is affected by our whole ecology: the things we can do for each other, the things the worlds of work and school can do, and the things the system can do for its citizens.
Professor Jim McManus, Director of Public Health, Hertfordshire County Council
NICE Quality Standard QS183
Physical activity: encouraging activity in the community
This NICE quality standard provides useful best-practice benchmarking for local authorities, healthcare commissioning groups, workplaces and schools. It covers how local strategy, policy and planning and improvements to the built or natural physical environment such as public open spaces, workplaces and schools can encourage and support people of all ages and all abilities to be physically active and move more.
- Statement 1 Local authorities and healthcare commissioning groups have senior level physical activity champions who are responsible for developing and implementing local strategies, policies and plans.
- Statement 2 Local authorities prioritise pedestrians, cyclists and people who use public transport when developing and maintaining connected travel routes.
- Statement 3 Local authorities involve community members in designing and managing public open spaces.
- Statement 4 Workplaces have a physical activity programme to encourage employees to move more and be more physically active.
- Statement 5 Schools and early years settings have active travel plans that are monitored and updated annually.
Figure 3: NICE Quality Standard. Physical Activity: Encouraging activity in the community (2019).
Work by the World Health Organisation (iii) has considered the complexity of factors that interact to shape a person’s physical activity behaviours.
Interventions that address any one part of this system in isolation are not likely to have substantial effects, but by carefully teasing out the important factors and how to influence them effectively, multifaceted interventions can be implemented that address a range of these factors and are able to increase the proportion of people who are achieving recommended levels of physical activity. Recent quality standards for physical activity from NICE (figure 3) support this view that many systems need to be addressed together to improve physical activity levels.
The evidence presented here is not comprehensive, but aims to present the story so far through selected high-quality research that the NIHR has funded into how to increase physical activity at different times in people’s lives, as well as through changes related to the workplace and the built and natural environments. We hope that this report increases awareness of the evidence to support different interventions, and can lead to more active and healthier communities across the UK.
A note about referencing
This review uses three forms of referencing: Summaries of featured studies use a number and can be found here. Ongoing and feasibility studies use a letter and can be found here. And where these or other publications are referred to in passing, the review uses roman numerals and can be found here.
Early years
Introduction
Our early childhood years are essential for development and are considered to have important and long-reaching consequences throughout our lives. Even before birth, pregnant women benefit from physical activity and, with sensible adaptation, this does not cause any harm (iv). Physical activity in infants and young children has both immediate and longer-term benefits related to physical health and motor development, as well as sleep, cognitive development and quality of life. Evidence of the benefits of physical activity for young children is growing, and the Chief Medical Officers as well as World Health Organisation (v) have developed guidelines. Compelling links are being made that more active pre-school children are likely to become more active school age children and adults (vi).
This chapter considers: what can we do to encourage and support infants and young children to enjoy being active from birth up to age four?
Research findings
There is relatively little evidence about how best to increase activity levels in young children. Although simple interventions around parental goal setting have been shown to be effective for some other behaviours, physical activity appears to be less readily influenced.
A large review of studies (Study 1) with children up to the age of six assessed the social factors associated with physical activity levels. It suggests that ways to encourage parental monitoring (where parents try to understand and supervise their children’s activities) are likely to be an important factor for increasing physical activity. The review also found that training providers, such as school teachers, could increase children’s levels of moderate-to-vigorous activity. Maternal role-modelling, where mothers are physically active with or without their child, showed promising results in the three studies that assessed it. Some other factors that might intuitively be expected to affect activity were not shown to make a clear difference, including the child’s gender, parental goal setting, social support, motor skill training, and increased time for physical activity. Although some important factors have been identified, there are likely to be others, and the interaction between combinations of factors may be crucial. This research has begun to unpick the influences on behaviours in young children, but additional work is needed to determine how best to modify these factors.
The preliminary Empower study (vii) involving mothers and infants attempted to change family behaviours to prevent obesity. This noted that while goals that were set around diet and sedentary time were mostly achieved, most of the unsuccessful attempts at setting goals were related to increasing physical activity. This suggests that a much better understanding of the factors relating to physical activity is needed, not only to reduce the proportion of people who are obese, but to improve the health of all infants.
Ongoing research
The ongoing Startwell project in Birmingham (Study A) has developed a nutrition and physical activity training programme for staff in nurseries to help them make the nursery a healthier environment for young children. The study will assess changes in the food and drink offered, opportunities for active play, and how staff model healthy behaviours. If this proves to have been effective, it could inform other programmes to train people who work with young children.
Evidence shows that being active as a child or young person can continue into being an active adult. Inequalities in activity can therefore become ingrained at a young age.
Michael Brannan, National Lead for Physical Activity, Public Health England
The NAP SACC UK feasibility trial (Study B) in 12 nurseries is evaluating how effective and cost-effective changes to the nursery environment can be for nutrition and physical activity. The trial adapted the US Nutrition and Physical Activity Self-Assessment for Child Care (NAP SACC) intervention, and implemented it in six of the nurseries, along with a home component for parents using digital media. The trial is looking at changes to nutrition, physical activity, sedentary behaviour, and oral health in nurseries, as well as goal setting and changes at home.
Conclusions
Research has not identified any single changes that in isolation have large overall effects for infants and young children. This is not surprising given the diversity and rapid development of children during these earliest years, and the competing pressures their parents experience. Many interrelated factors and activities contribute to children’s physical activity, and to their time spent being sedentary. To help infants and children be more active will require many small changes throughout the whole variety of places and activities that make up a child’s day. Even where young children attend nurseries, their family and physical and social environments are likely to be particularly important influences on the physical activity of infants and young children.
Prompts for reflection
- How can parents and families be encouraged to increase physical activity during early years?
- What support do we give nursery and pre-school providers to promote enjoyable, active play?
- How are local green spaces designed and managed to meet the needs of infants, children, and families
Children of primary school age
Introduction
The greater children’s physical literacy (confidence, competence, understanding, knowledge, and - most importantly - enjoyment) the more active they are likely to be. However, many children begin to reduce their physical activity when they begin school, and girls and those from less affluent families are less likely to enjoy being active (viii). Schools are promising places to deliver interventions to increase physical activity, providing a means to deliver interventions to large numbers of individuals at once, as well as to shape the school environment and culture. But schools are also places where children are often encouraged to sit for long periods. How can we encourage children aged 5 to 11 to be more active travelling to school, in the classroom, during breaks, and outside school?
Research findings
Research has explored how physical activity could be encouraged at school. One large trial (Study 2) found that that a school programme (including teacher training, lesson planning, homework tasks involving parents, and written materials for parents and newsletters) did not change overall physical activity or sedentary behaviour in the short term or a year later. The study, with 9-10 year olds in 60 schools in England, used accelerometers to accurately measure activity levels and provide more complete and objective measures of activity than diaries or recollections. The researchers speculate that the reason they did not see a change in activity may be that intervention ‘dose’ was not high enough, and it is possible that a more intensive version of the same set of interventions could be effective. The intervention did appear to improve other behavioural outcomes, reducing weekend screentime by 21 minutes per day, reducing snacking,and reducing consumption of high-energy drinks.
Children and young people are not independent individuals so our approach must recognise the importance of their family, and their physical and social environments such as schools and neighbourhoods.
Michael Brannan, National Lead for Physical Activity, Public Health England
A systematic review of quantitative and qualitative studies looked at research and experience of implementing health promotion programmes in schools in the UK. (Study 3) It aimed to identify those characteristics of programmes, schools or communities which make health promotion programmes more feasibly or sustainably deliverable in both primary and secondary schools. The review found that when preparing for implementation, important factors were consulting with parents and teachers, particularly when the initiative and its benefits are not already well known within the school, engaging pupils’ interest and attention, and identifying potential shared benefits for teachers and pupils. There is weak evidence that it is important a programme has a good ‘fit’ with the school, complements the school ethos, and fits with other activities. The initial implementation stage was more successful where changes were actively supported by school governors and senior staff, where there was a named co-ordinator of the programme within the school who was able to influence others, and where those delivering the programme received support with personal and professional development. Little research was available for the authors to derive clear recommendations about how best to sustainably embed a programme into routine practice, or the factors that affect whether a programme is implemented as intended, and when and how programme adaptation is justified (for example without undermining effectiveness).
A trial of the novel Healthy Lifestyles Programme for 10-11 year olds in 32 schools (Study 4) found that a healthy lifestyles week with drama sessions and goal-setting activities over the summer, followed by reinforcement activities during term, successfully engaged pupils across the socioeconomic spectrum, families and teachers, but did not result in changes to accelerometer-measured physical activity, food intake, or measures of obesity at 18 or 24 months, although children did reduce their unhealthy snacking. There were high rates of follow-up and the intervention was delivered as intended (both in terms of content and quality of delivery) leading the authors to conclude that it is unlikely programmes targeting a single age group can ever be sufficiently intense to affect weight status, and call for approaches that affect the school, the family, and the wider environment.
A large review (Study 5) found three studies that evaluated playground improvements in UK primary schools, but some methodological concerns were identified, meaning that the evidence generated is not strong. One study improved structures and developed three playground zones for sports, for fitness and skills, and for quiet play. It showed improvement in some markers of accelerometer-measured physical activity at 6 months and 12 months, with greater benefits for younger children. The other two studies improved playground surface markings. One did not find any change in measures of physical activity, while the other found an immediate increase in markers of physical activity. The popularity of The Daily Mile initiative (where all pupils are encouraged to walk or run for an additional 15 minutes during the school day), indicates that even basic outdoor spaces can bring important opportunities for physical activity. Beyond schools, a study in Blackpool (Study 6) has found that continued subsidies for free swimming led to an additional 33 swimming sessions per 100 children, and six per 100 children swimming at least once per year with the greatest effect seen among children aged 10-14. This indicates that removing the cost of swimming for children is effective in a very deprived local authority area, and the data suggest the effect may be greatest for moderately deprived groups.
Ongoing research
Beyond time spent being active, interventions to reduce sedentary time are also likely to bring health benefits. The ongoing CLASS PAL study (Study C) in 9-10 year olds is assessing a suite of measures that teachers are encouraged to use to adapt the way lessons are taught and how the school day is organised, with a view to breaking up sedentary time and incorporating more physical activity throughout the day.
The FRESH intervention (Study D) is a pilot family-based physical activity programme for children. The intervention is targeted at whole families, delivered at home with web-based tools. The study is predominantly recruiting from rural areas, where physical activity levels in children have been seen to be lower and to decline with age more rapidly than in urban areas. Noting research that youth physical activity promotion is largely school-based and of limited effectiveness, the FRESH intervention is attempting to involve family members who they consider likely to be crucial for long-term changes in physical activity.
Stand Out in Class (Study E) is a pilot trial to reduce sitting time in 9-10 year old children. It has set out to assess how effective height-adjustable desks are to reduce sitting time for children on an average school day, and how this may improve health, well-being and learning. A feasibility study found that sit-stand desks in a classroom for nine weeks reduced sitting time by 80 minutes/day. A pilot study is in now progress with Year 5, where the pupils use this type of desk in turn, for about one hour per day each.
Action 3:30 (Study F) is a feasibility evaluation of a programme to support teaching assistants to lead extracurricular physical activity sessions for 8 to 10 year olds. The intervention is based on self-determination theory, which suggests that teachers can develop pupils’ autonomy, belonging, competence, enjoyment and motivation in order to increase uptake of the sessions.
Conclusions
Evidence for how to increase physical activity among primary school-age children suggests that delivering health improvement interventions to children should be done both at school and at home. To increase physical activity further, research into acceptable ways to deliver higher ‘doses’ of interventions throughout pupils’ day, to make their school and home environments more conducive to physical activity, and to increase the involvement of families may be needed.
Prompts for reflection
- What could you do to enhance school buildings and playgrounds to increase physical activity?
- How can we encourage walking and cycling to school, through changes to the environment, and support to parents, carers and schools?
- What opportunities are there for schools to work with pupils and parents to find ways to increase physical activity?
Young people of secondary school age
Introduction
For young people of secondary school age, physical activity improves physical function and bone strength, as well as mental wellbeing (ix). Muscle and bone strengthening and balance activities during adolescence are particularly important in order to maintain function and good musculoskeletal health in later life (x). The government recommends that physical activity should take place both within and outside school (xi). However, only 20% of UK teenagers meet physical activity guidelines. Relatively little is known about how to motivate teenagers to change and sustain these behaviours (xii), although physical activity literacy, and particularly enjoyment appears to be important (viii). This is also an important time for establishing patterns of behaviour that can sustain health through adulthood and old age. During secondary school, from age 11 to 16, people’s social circles expand and take on increasing importance, and much of the research addresses social influences on physical activity.
A review of 13 interventional studies (xiii) did not find that changing activity levels affects cognitive function, although the two were associated. Importantly, the review did not find that allocating school time to physical activity compromised academic achievement.
Research findings
Interventions for older children and young adults have demonstrated some ways to increase physical activity, and theories about which approaches are more effective have been developed and tested. Giving young people some responsibility to decide on and make changes to improve health may be one effective way forward.
A 2013 Cochrane systematic review of international research (not funded by the NIHR) (Study 7) noted that there is some evidence that for adolescents, school-based interventions can increase physical activity. The interventions increased time spent physically active by 5-45 minutes/day, reduced sedentary television time by 5-60 minutes/day, and increased VO2max (a marker of cardiorespiratory fitness). However, the review’s findings were limited by the quality of the included studies, and the reviewers noted that additional research on the long-term impact of these interventions is needed.
A large review (Study 5) of studies into improving health in schools in the UK and abroad found that empowering students to modify their environment was effective in increasing general health outcomes. Two of the studies assessed interventions in US middle schools (ages approximately 11-14 years) to change the school food and physical activity environment. These independent studies were well conducted though still at some risk of bias, involving 8 and 12 schools in the intervention arms. Both improved some measures of physical activity, but not of dietary quality. One found promising effects with regard to reductions in aggressive behaviour, and the other noted that pupils became more able to influence their schools to create environments supportive of physical activity. Altogether, there was non-definitive evidence for the effectiveness of interventions in the school environment to build communities and relationships, and to empower students in modifying food and physical activity environments.
This review also identified a number of particular theories which could be helpful for developing effective interventions, and assessed evidence for their effectiveness. It found that interventions based on three types of theory, all of which contain strong social aspects, were more likely to be effective. Key implications were: schools are more likely to encourage healthy behaviours if they provide opportunities to participate in school life, develop the skills necessary for this participation, and enable students to gain recognition for this; schools with stable student and staff bodies, good relationships between staff and students, and an ethos of shared norms, are likely to have better health outcomes; schools should develop practical reasoning about pupil’s own and others’ feelings, perspectives, and emotions, increasing the ability to form strong relationships
It’s essential to see beyond organised, competitive sport so as to reach people who don’t see themselves as sporty. Physical activity needs to be built into all areas of children and young people’s lives.
Philip Insall, Public contributor
The Bristol Girls Dance Project (Study 8) was a project to increase physical activity in adolescent girls, a group at high risk of inactivity. The features of the intervention were carefully developed with stakeholders during formative work. The study delivered dance classes to girls in several schools twice a week for 20 weeks, and measured their activity levels throughout the day. It did not find that twice-weekly dance classes increased overall physical activity, and it may be useful to consider why. One important factor may have been that girls in the trial were recruited when they were new in their school, and so had not settled into a routine of particular activities. Many of the girls may have dropped out as part of the process of exploring alternative activities. The study found that the girls who opted to attend the classes were those who were already relatively active compared to those who did not opt in. The researcher team speculates that if the intervention had been implemented once the girls were better established in the schools, rather than when they first arrived in Year 7, it may have been possible to proactively recruit those who were less active, and ongoing attendance at the dance classes may have been higher.
The introduction of free bus passes for young people in London led to an increase in journeys by bus. This evaluation (Study 9) also found that travel-diary surveys did not demonstrate a change in overall numbers of journeys by walking or cycling. This suggests that improving public transport does not displace walking. The evaluation used surveys and was not able to assess the incidental physical activity associated with these increased bus journeys, such as walking to and from bus-stops, or the increased opportunities for active recreation the transport provided. As the bus passes did not reduce other walking journeys, they are likely to have a positive effect on physical activity overall. More detailed and objective evaluations of the effects of interventions to increase access to public transport would help to quantify these benefits.
The Girls Active study (Study 10) supported schools to improve their physical activity culture and practices. Teachers attended training, were provided with resource packages, and then developed action plans that considered girls’ motivations and ways to increase participation in sport and physical education. The teachers then selected and developed peer leaders from among 11-14 year old girls, who in turn encouraged others to be more active. Objectively measured activity after 14 months was assessed, but not found to have changed. The authors suggest several reasons for the lack of effect. It may have been due to the long time for schools to set up the programme, and a disconnect between the plans for activities and those actually undertaken. Peer leaders may not have had the maturity and skills to influence their peers, particularly where there were conflicts with other school commitments. They suggest that a school culture shift is necessary, with involvement of pupils, teachers, and senior leadership, and that this sort of change may take several years to develop.
Ongoing research
Engaging adolescents in changing behaviour (EACh-B) (Study G) will evaluate a three-component intervention including: LifeLab, a three week science module to motivate and support pupils to think about how lifestyle changes at an early age can affect their health and the health of their future children; encouragement from trained teachers to improve diets and exercise; and a smartphone app involving friends and using game features.
An ongoing study (Study H) is assessing how and why young people from a deprived town in Cornwall engage with a long-running dance group, the TR14ers. It will assess physical activity, diet, nutrition knowledge, emotional well-being, and other health-related behaviours. The research also seeks to understand how and why young people engage and sustain engagement with the group and the impact of participation on health and the wider determinants of health in the short, medium and long term. It will enable researchers and practitioners to understand how to create the conditions to engage and sustain participation in health promotion programmes in areas of high economic deprivation.
The GoActive intervention (Study I) for 13-14 year olds aims to increase daily physical activity. The intervention actively encourages pupils who may be shy or less active to participate. Each class chooses two activities each week from a range chosen to appeal to a wide variety of students, and are encouraged to try at least one by mentors and peer leaders. Key themes of GoActive are: choice and novelty of activity; mentorship from older pupils and peers; competition and reward with a points system for participation; and flexibility of times and locations to suit pupil preferences.
The trial of Peer-Led physical Activity iNterventions for Adolescent girls (PLAN-A) (Study J) will train 13-14 year old pupils over three days to be peer supporters. These peer supporters will informally diffuse health promotion messages to their peers in order to encourage physical activity. The intervention is based on two main theories: the Diffusion of Innovations theory (about how ideas, beliefs and behaviours are socially communicated), and Self-Determination Theory (about how to foster high-quality and sustainable motivation). Physical activity outcomes will be measured with accelerometers, and cost-effectiveness estimated from a public sector perspective.
Conclusions
Developing new skills, such as dance, could have short and long term benefits that are not necessarily captured by changes in total moderate-vigorous physical activity, or even with cardio-respiratory fitness. One-off interventions to increase organised physical activity may be effective for young people, but once the activity or programme finishes, there is too often little to prevent their reverting to previous patterns of physical behaviour. Ways to sustain changes in behaviour are needed.
To significantly increase the proportion of children and young people meeting guidelines for physical activity will require changes that not only encourage deliberate activities such as sport, but that build incidental physical activity into all areas of children and young people’s lives, while also breaking up sitting time. Small changes that build increased activity into many routine activities, and that carefully take account of the social environment appear to be promising approaches. These diverse opportunities can provide valuable activity in themselves and, if they can improve young people’s confidence in their physical abilities, may also make them more likely to engage in other activities.
Prompts for reflection
- When young people begin secondary school, are they supported to take part in a wide range of physical activity opportunities in and outside school?
- How can we encourage more active travel for all young people?
- Are there additional barriers for certain groups? What initiatives could encourage young people to avoid sitting for long periods
Adults
Introduction
This chapter considers adults, from leaving school up to their mid-60s. Some people continue to engage in structured exercise or sport throughout adulthood, while many are physically active only incidentally as part of their routine day, and over five million (xiv) feel unable to be physically active at all. Physical activity plays a key role in the maintenance of good health and reducing the development of many diseases. Systematic reviews have begun to identify and collate the active ingredients that make interventions likely to be effective for different groups. For example, one meta-analysis (xv) found that interventions for inactive adults are more likely to remain effective after at least six months where they used: action planning, instruction on how to perform the behaviour, prompts or cues, behaviour practice or rehearsal, graded tasks, and self-reward.
Ageing of adults is not uniform, with those in poor health or poverty having very different experiences. The greatest health gains are likely to come from modest increases for those who are least active, and from interventions designed to be sustained in the long term (xv). This suggests a significant role for adaptations to encourage activity as an inherent part of people’s day, whether through leisure, travel, work, or reducing time spent sitting. Despite nearly two-thirds of the adult population meeting the CMO physical activity guidelines (xvi), stubborn inequalities remain. Women, those from lower socio-economic groups, and black and South Asian communities are less likely to be active.
Research findings
Some interventions have attempted to increase levels of incidental physical activity as adults go about their daily lives. The relative benefits of moderate to vigorous physical activity compared to light activities or even simply standing are not well explored. One review (xvii) noted that, while workplaces and many urban areas may not be suitable for vigorous physical activity, it may be relatively straightforward to replace sedentary behaviours such as sitting with standing or light activity. For example, many people could benefit if buildings are designed to encourage movement, people are encouraged to stand on public transport, and standing desks are available in offices. These changes would make few demands on individuals and could shift population activity patterns from being sedentary to including significant amounts of standing or light activity. This may bring its own health benefits, and may also make any later transition to moderate or vigorous physical activity more likely to be successful.
A study of factors from early adulthood that influence mid-life physical inactivity (Study 11) found that people who are obese in early adulthood, or who live in industrial or local authority housing areas are more likely to remain inactive or become more inactive, and less likely to become regularly active.
Interventions may need to be tailored carefully to these groups in order to be effective and reduce inequalities. Interventions to increase physical activity as part of reducing other health risks have been shown to be effective in the short term and sustainable in the long term. The Football Fans In Training programme (Study 12) was intended as a weight-loss programme for men. To address diet and physical activity it used behaviour change methods such as goal-setting, self-monitoring, and feedback. Coach-led physical activity training and encouragement of mutual support and learning were central. These behavioural changes were notably well sustained, and even three and half years later, participants continued to walk for an extra 90 minutes each week. Important features that may have contributed to the sustained effect of the intervention include the continued self-monitoring of diet and physical activity and the social support networks that were developed. It is also likely that using professional sports grounds to deliver the intervention may have increased participant buy-in and motivation.
The Walking Away from Type 2 Diabetes trial (Study 13) delivered a three-hour structured group education programme with pedometers to patients with high risk scores for developing diabetes. The intervention addressed self-efficacy (belief in one’s own ability to succeed at a task), identified barriers to walking, promoted self-regulatory skills through action planning and pedometer use, and encouraged individuals to increase their physical activity by 500 steps/day every fortnight, up an additional 3000 steps/day. The intervention was low resource, and found a moderate increase of 411 steps/ day at one year. However, the difference was not sustained in the longer term. Participants with more abnormal glucose measurements at baseline were more successful at changing their behaviour at one year. This suggests that the process of individuals plotting their glucose values on a risk chart may have increased these patients’ perception of the severity of their disease and so increased their intention to be physically active. In contrast, the 23% who did not attend the initial education session and refresher sessions had higher BMIs, larger waist circumferences, were more likely to smoke, and may have been more likely to come from deprived areas. This suggests that additional strategies and personalised approaches to support uptake and adherence to prevention programmes may be particularly useful for these groups.
An evaluation (Study 14) of exercise referral schemes, where doctors refer a patient to a fitness programme, found that referral uptake was lower for people without their own transport or from more deprived neighbourhoods. This suggests that good transport links to such programmes are important, and it may be that enhanced public transport could improve uptake from more deprived areas. Where people were referred because of cardiovascular risk factors, their uptake was greater, which may reflect increased motivation and strong belief that exercise is an effective way to reduce this health risk. This review did not explore the specific aspects of interventions that make them more effective. A separate economic assessment of exercise referral schemes (xviii) found that although no clear changes were seen in physical activity, the schemes may have improved quality of life. What evidence is available indicates such referral schemes are likely to provide reasonable value for money based on health outcomes, particularly in those who are obese, have high blood pressure, or have depression.
Use of graded tasks, where large tasks are broken down into smaller, more manageable ones, may be particularly effective. One primary care study (Study 15) provided a pedometer and 12-week walking programme based on behaviour change techniques to encourage building long-term habits, with advice to gradually add 3000 steps in 30 minutes. A year later, participants had significantly increased their daily step count by 10% and their moderate-to-vigorous physical activity by one third. These changes were sustained at three years. Whether this intervention was delivered by post or through practice nurse-led support groups made little difference, suggesting that significant professional support may not always be required. The postal intervention was also more cost-effective. By monitoring steps using pedometers built into smartphones, it is possible that the costs of the intervention could be reduced further.
A review of the barriers to physical activity participation in mid-life (Study 16) emphasised that consideration of these barriers is important for tailoring interventions to particular groups. Interventions that improve psychological factors of motivation, self-belief, and self-esteem may be important. The review also identified that people are deterred from opportunities for physical activity by cost. A trial (Study 17) offering subsidised activities to residents in Devon slightly increased residents’ time spent being physically active, but did not show an increase in numbers of people meeting physical activity guidelines. The authors noted that this lack of effect may have been because few residents had been aware of the interventions.
A different evaluation (Study 18) examined the impact of variations in local authority pricing policies on health inequalities. It found that offering universal free access to leisure facilities, alongside significant marketing and outreach activities, led to an additional 4% of the local population attending gym or swim sessions in a month and increased overall levels of self-reported physical activity levels by 2 percentage points. The effect was greatest for more deprived groups. Together, these studies indicate that reducing cost barriers and increasing community engagement may be important for making all residents more active, particularly those who received out of work welfare benefits, low wage households, working families with young children, and retired people.
Taking part in environmental and conservation activities is sometimes considered an effective way to encourage people to be physically active. However, a systematic review (Study 19) found that most of the research in this area was of low quality, and so could not draw definitive conclusions. Most of the studies did not find significant effects on health and well-being. Some studies did suggest benefits for self-reported health and physical activity, but an increased risk of anxiety. Participants enjoyed the social opportunities afforded by these programmes.
A review of UK guidelines (Study 20) found little specific guidance for how effectiveness of interventions varies between ethnic groups, nor how they can best be adapted. The development of a more fine-grained understanding of the factors affecting physical activity is important for effective interventions. The scarcity of ready-made advice about how to tailor interventions to particular groups increases the importance of undertaking detailed local assessment of barriers to physical activity for a wide range of groups, and the need for effective community engagement to shape interventions and raise awareness of opportunities.
Ongoing research
The Yoga Study (Study K) is working with people of South Asian descent, who have elevated risk of type 2 diabetes and cardiovascular disease. This group may be less likely to engage in physical activity, and the study has identified culturally appropriate forms of physical activity. They are testing whether yoga and light intensity walking are effective in reducing type 2 diabetes. A novel diabetes prevention programme (Study L), has found that people with existing type 2 diabetes could be recruited and trained in a range of techniques to become peer supporters for participants at high risk of themselves developing type 2 diabetes.
The NIHR Public Health Research Programme is commissioning further research into which interventions are effective to maintain or increase physical activity for people in mid-life, with particular attention to factors such as ethnicity, socioeconomic status, occupation or gender.
Conclusions
Physical activity in adults tends to reduce with age, but these studies have indicated there are effective ways to help adults to become more active. Many studies have found that a variety of techniques are suitable to help adults to maintain changes in their behaviour over several years. People are becoming increasingly aware of the benefits of physical activity, and the challenge is not only to provide opportunities for physical activity, but to further increase people’s motivation and capability. People for whom sport and other physical activity does not appeal are likely to have most to gain from appropriately tailored interventions, and surveys (xvi) have found that although the number of adults engaged in traditional sport are stable, people are increasingly taking up activities that can fit into a busy day, that are enjoyable, and where ability does not matter.
Prompts for reflection
- Beyond sport, what can be done to achieve modest improvements in everyday activity?
- What can we do that will appeal particularly to those who are least active?
- What are the most important active ingredients you could consider including in order to make your interventions as successful as possible?
Workplace changes
Introduction
It makes sense for organisations to encourage employees to keep active. The links between activity and health and well-being means that workplaces which support staff to stay active are likely to be rewarded by greater productivity and lower absence rates. Long periods of sitting still can lead to poorer health, from cardiovascular disease to diabetes and musculoskeletal problems, yet people may feel restricted to certain postures as they complete tasks. In this way, there is a clear business case for workplace interventions to support and maintain exercise and activity among employees. In research terms, there are also advantages to workplace activity studies. These involve well-defined populations where interventions can be tested and evaluated in more controlled settings. However, workplace interventions will do little for those who are not in work, and interventions for people in office-based jobs may need to be very different to those whose jobs are active or require significant standing. A diversity of interventions in different contexts will always be required to address inequalities in physical activity.
Many employers recognise that they have an obligation to the health and well-being of their workforce. Investing in the health of employees can also bring business benefits such as reduced sickness absence, increased loyalty and better staff retention. NICE Guideline PH13 (2008), Physical activity in the workplace.
Research findings
We know more now about the harmful effects of extended periods of sitting. A Cochrane review (Study 21) identified studies of different kinds looking at interventions to reduce sitting time at work. This included ten studies looking at sit-standing desks which reduced sitting time but evidence was low quality and effects were less marked when people were followed up for longer. Other low quality research found mixed results from changes in workplace policy (such as introducing structured breaks) or practice (such as computer prompts to walk about the room, activity trackers, and treadmill desks). Most studies in this review were small with a high chance of bias, and the findings may not apply to non-office workers. A subsequent trial in hospital office staff (Study 22) tested a multi-component intervention involving group education, sit-stand workstations, behavioural feedback, goal setting and action planning, brief one-to-one coaching as well as a self-monitoring and prompt device. This intervention aimed to reduce sitting time at work. The intervention group reduced their sitting time at 12 months, with a difference of 83 minutes per work day seen between the intervention and control group. Sitting time was mainly replaced by standing time, and so stepping time did not change. Additional benefits in work-related and psychological health were seen. Although the NHS is a large employer, it is not certain how generalizable these results will be for non-NHS settings, nor how best to encourage more stepping as opposed only to standing. Many outcomes of interest related to health or workplace absenteeism will be assessed in a large follow-on trial on council workers with outcomes measured over two years.
A loyalty card scheme to improve maintenance of physical activity changes in office-based employees was evaluated in Northern Ireland (Study 23). It used key fobs that could be tapped on sensors placed within 2 km of workplaces to earn points that could be redeemed at local retailers. Motivational emails, tailored feedback, and information about walking routes were also supplied, and participants were encouraged to set their own goals, monitor their activity, and develop prompts. Unfortunately, the workplaces underwent significant restructuring during the evaluation, which may explain why the intervention group decreased their physical activity compared to the control group. Other possible reasons for this unexpected decrease in physical activity are that the incentives were not sufficient (only 39% were redeemed), and that early technological difficulties left participants feeling frustrated. The authors also consider whether the use of financial rewards to change health behaviours may have ‘crowded out’ intrinsic motivation (a person’s interest or enjoyment in the activity itself) to be active, but conclude that this was not the case.
Ongoing research
A collaboration between public health, built environment and computer science researchers (Study M) is examining how the indoor layout of UK office buildings affects physical activity and sitting time.
Initiatives to reduce sitting time in offices include a small feasibility study (Study N) which assessed the impact of sit-stand desks at work on energy expenditure, sitting time, and cardio-metabolic markers over 3 months. It found that most workplaces could accommodate sit-stand desks, and these were well received by most participants, and sitting time was reduced by an estimated hour and a half per day. The study did assess the most common reasons people reported switching from sitting to standing (back ache and stiffness, returning to the desk after being away, and feeling guilty), and for switching from standing to sitting (tiredness, leaving desk, and type of activity).
The UP FOR 5 study (Study O) is investigating whether an intervention to reduce total sitting time and to increase movement breaks throughout the day can improve health markers in people who are a high risk of developing type 2 diabetes.
Stand Up For Health (Study P) is a feasibility trial of an intervention for contact centre staff. The intervention is co-produced with employees, offering tailored activities. Outcomes of interest will be mental well-being, musculoskeletal disorders, productivity and job satisfaction.
And a large trial of the SMART Work and Life intervention (Study Q) follows on from study 31. It will be the largest trial of its sort, with the longest follow up. Council office workers will be followed for two years to see how effective standing desks and a programme of behavioural change interventions are at reducing sitting time, physical activity outside working hours, and a variety of biochemical and psychosocial measures.
Another trial (Study R) is examining the effectiveness of providing booklets, pedometers, walking routes, and goal setting support to employees in order to increase walking during their commute.
Beyond office workplaces, the SHIFT Study (Study S) is evaluating a structured health intervention for long distance truckers to change physical activity, sitting, and diet behaviours. An education session, physical-activity tracker, and simple exercise equipment for a ‘cab workout’ will be provided. Outcomes will include measures of physical activity, sitting time, sleep duration, and health markers relevant to cardiovascular risk.
Conclusions
The majority of working age adults spend much of their waking time at work. There is an opportunity for employers and workplaces to support staff to be more active. This is important given the links between activity and health, well-being, and productivity that are well established for those in sedentary jobs. Recent NIHR research has looked at different approaches taken in the workplace. A trial of standing desks in a hospital showed sustained reductions in sitting time, which supported evidence from a previous review. But types and patterns of work vary widely, and effective interventions will need to be developed and tailored to account for this. Carefully designed and evaluated interventions helps us to understand more about the complex interplay and drivers which encourage people to keep active over time. Qualitative feedback from study participants has suggested that efforts to develop more healthy habits in one area of life, such as reducing sedentary time, are likely to prompt efforts to improve other areas, such as diet and physical activity.
Prompts for reflection
- Could we introduce adjustable desks or other ways to reduce long periods of sitting?
- Does your workplace have the necessary facilities and systems to encourage active commuting?
- How can the case be made effectively to employers that they should support more physical activity?
Older adults
Introduction
We know from good evidence that physical activity can help people to maintain their functionality, independence, and quality of life, preventing and delaying some of the diseases which affect people as they age. These range from osteoporosis to cardiovascular disease and cognitive decline, as well as the syndromes which together can be described as frailty. Improving strength and balance is particularly important to reduce falls, which are a common injury for older people and may lead to people no longer living independently at home. And yet older people tend to be less active – with 47% of people aged 75-84 being inactive, and 70% of those over 85 years. Over half of all inactive people in England are aged 55 and over (xiv). As well as the benefits of improved strength, balance and overall fitness, activity can also be an important way of reducing isolation and increasing well-being for older people.
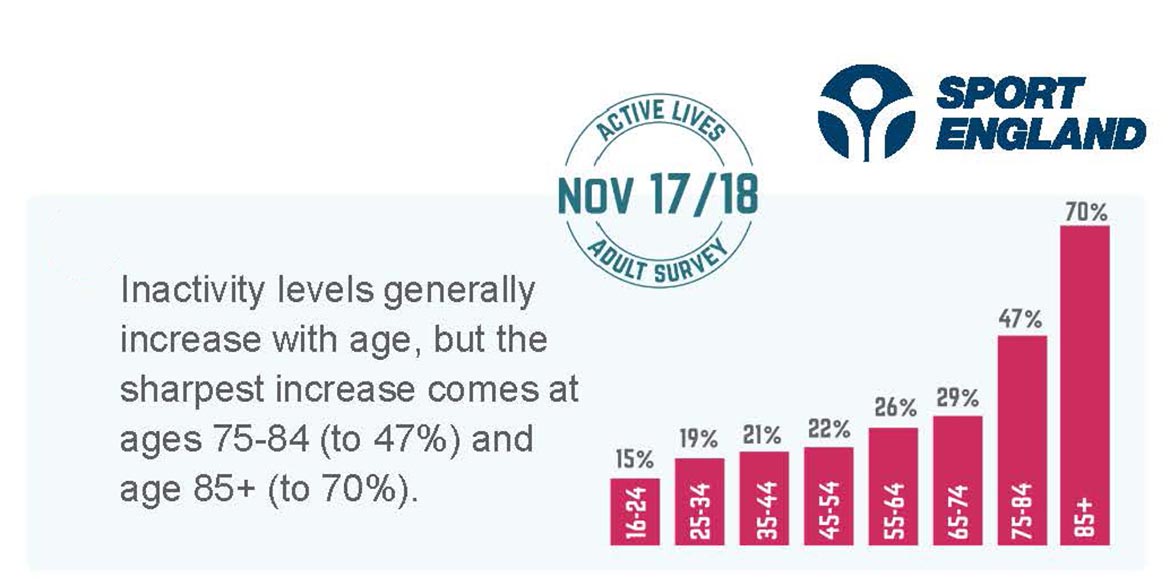
Figure 4: There is a sharp increase in the number of people becoming inactive from age 75. Sport England (xiv)
Research findings
There appear to be very few research studies looking particularly at transitions to retirement, according to one review (Study 24). This may be an important time of transition in which to intervene, and could benefit from further research. However, a number of attempts have been made using different approaches to get older people to be more active at home and in the community. NIHR research has looked at some of these interventions to identify lessons for individuals and decision-makers.
Evidence suggests that a range of approaches may be effective in promoting exercise in older people, including both supervised exercise, from walking groups to dance classes, and behavioural approaches such as motivational counselling and tailored activity plans. A review of reviews, (Study 25) looked at a number of questions relating to physical activity in older people, including what works in increasing activity levels and reducing barriers to participation. Evidence was mixed on the duration needed and the added benefit of input from activity professionals. Available evidence suggested that older people were more likely to keep exercising with group classes in a centre than through homebased activity. Although research often didn’t follow up older people for any length of time, evidence in this review suggested the need for interventions to combine supervised exercise opportunities with theoretical understanding of behaviour change to sustain increased activity over time. Another part of the review looked at nine qualitative reviews to understand barriers to exercise. These included previous exercise habits and health status as well as personal and cultural preferences. These findings have contributed to advice (xix) from Public Health England about how to improve the uptake and maintenance of healthy behaviours in older adults to promote cognitive health.
Similar messages came from another review of ways to get older people more active. Evidence supported use of interventions, from walking groups to pedometers and motivating people to exercise more.
Walking appeared an important activity for this age group. Qualitative research on attitudes to exercise highlighted issues of identity in relation to exercise, fears of hurting oneself or falling and the importance of social aspects of activity. A synthesis of qualitative studies also showed the added social benefits of exercise, but few interventions were designed with this in mind. (Study 24)
Evidence from one large trial found that attending a weekly exercise class led to more people reaching recommended government activity levels of at least 150 minutes a week, but no difference in those doing exercise at home. The exercise class resulted in significantly fewer falls, a frequent cause of injury and loss of independence, although it did not find other direct changes in health and well-being. The trial involved over 1200 older people from 43 general practices. For six months, people took part in weekly exercise classes, home-based activity or normal care with no particular exercise plan. Their activity levels were measured a year after the intervention ended. Researchers noted that groups who were least active at baseline were also the most likely to drop out of the study. (Studies 26 and 27).
A further study as part of this trial looked more closely at the characteristics of those who had maintained and improved activity levels. They found lowest rates among the oldest in this age group and women. Perhaps not surprisingly, the people most likely to achieve recommended activity targets were those who were already physically active and more fit and had wider social networks. This suggests the need to actively target approaches at certain groups in future interventions.
This is reinforced by important trend data from the ELSA project (xx) (part-supported by NIHR) which looks in detail at populations of older people over time. This showed that a greater proportion of older people are inactive now compared to ten years ago. It also found that this was more true for certain people, including women, smokers and those with a longstanding illness, depressive symptoms, arthritis and who were obese. This suggests the need for more tailored approaches to get these people active.
A successful example of a tailored approach is the PACE-UP study (Study 15), a pedometer intervention based on the older person’s own baseline step-count, which increased both frequency and intensity of walking in a graded manner in primary care patients aged up to 75 years. It demonstrated significant safe and sustained increases in both step-counts and time in moderate-to-vigorous physical activity levels at 3 years.
...by encouraging, facilitating and supporting people to take part in enjoyable physical activity throughout the lifespan and health-span they can be helped to feel better, delay the onset of disability, frailty and dementia and can achieve what most people want to achieve: mainly to have a social life, and to stay in their own homes.
Professor Sir Muir Gray, Consultant in Public Health Oxford University Hospitals (xxi)
Ongoing research The REtirement in ACTion study (REACT) (Study T) is assessing the effectiveness and cost effectiveness of a community-based physical activity programme to help high-risk people over 65 to remain mobile. It uses a 12 month programme, with initial individual assessment and twice-weekly hour-long sessions to for six months, followed by ongoing exercise sessions, signposting to local activity opportunities, and the option to become ambassadors for the programme.
The Walk with Me Study (Study U) is a feasibility and pilot study of a peer-led walking programme for inactive 60-70 year olds. Initial findings were that the intervention was acceptable to participants and appeared to increase physical activity at 12 weeks and 6 months. The authors noted the need to tailor recruitment for very inactive, less healthy participants, and males.
Chair based exercise programmes may be beneficial for older people who find usual exercise programmes too strenuous. An ongoing feasibility study (Study V) in day centres, care homes, and community groups is assessing how feasible, acceptable, and tolerable chair based exercises are in these settings.
Developing the idea that social aspects of interventions are important, Project ACE (Study W) is assessing the use of peer volunteers to promote active ageing in order to identify the best bet physical activity promotion strategies for older adults.
Conclusions
Our population is ageing, and people tend to be less active as they age. Research shows that interventions such as walking groups to encourage activity are effective, with the most impact from classes and group activities, and more moderate effects seen with home-based individual approaches. To sustain benefits, interventions appear to need components that are based on theories of behaviour change, such as motivational counselling and goal setting. We don’t know enough from the research about the kind and intensity of intervention which works best, but qualitative evidence suggest the importance of social aspects of exercise, and reassurance around safety and health beliefs. More effort needs to be directed at certain groups most likely to benefit and least likely to take part in initiatives, including those with lower starting fitness and health problems or with weaker social networks.
Prompts for reflection
- What are the most important life changes that influence physical activity in older people?
- Can local physical activity programmes be adapted for people who are less able because of injury or health conditions?
- Are physically active social and group-based opportunities available for older people
Changes to the built and natural environments
Introduction
Changing our environment and the cues it provides can be a powerful way to shape behaviour and increase physical activity. For example, transport policy interventions can bring both advantages and disadvantages for physical activity. They may promote active travel or improve access to opportunities for recreation and exercise. Measures to increase motor traffic capacity can effectively dissuade walking and cycling, as well as worsening air quality. Large roads can also act as barriers to non-vehicle travel, cutting communities off from each other as well changing the flow of traffic and potentially discouraging walking or cycling. Although many interventions have focussed on active transport, environmental approaches often benefit many groups on other ways: changes such as leisure opportunities, good paths, benches, and public toilets make towns and countryside easier and more accessible for everyone, older and younger alike. Interventions can generate a wide range of co-benefits, improving many aspects of our environment and health.
Research findings
Chapter four established that characteristics of neighbourhoods where people live in early adulthood can have strong and persistent influences on physical activity. In Chapter three, we saw that providing free bus travel to adolescents increased their use of buses without displacing walking or cycling. However, that study did not assess the physical activity associated with bus journeys. Several studies have looked more closely at the effects of transport interventions and the built environment on physical activity.
Almost any intervention to make the environment more conducive to active travel will mean increased physical activity – but also better air quality, fewer road casualties, improved social cohesion, lower climate emissions, and less noise.
Philip Insall, Public contributor
Following introduction of a 22 km bus lane with an off-road path for walking and cycling, an evaluation (Study 28) found that residents near to the busway increased the time spent actively commuting, were more likely to commute by bicycle, and reduced the number of trips by car. This increase in physical activity on the journey to work appeared to be greatest for those people who were least active at baseline.
In contrast to the busway, new urban motorways may have the opposite effect if they do not sufficiently consider walking, cycling, and public transport. An evaluation (Study 29) of a new motorway in Glasgow found that people living near to the motorway increased their car use, but did not increase their active travel and may have reduced their overall physical activity. Some people felt cut off from other local people and places, and health outcomes for local communities may have been harmed.
These studies indicate the importance of well-designed transport systems and built environment layout. Large infrastructure projects bring significant opportunities to improve physical activity and well-being of those living nearby. Although changing road systems is expensive, where roads are being built or changed for other reasons, the inclusion of additional facilities to encourage active commuting may carry relatively low costs.
Transport infrastructure should be able to adapt to changing patterns of use over time, and by different groups of people.
The Olympic Games in London in 2012 offered an opportunity to assess (Study 30) whether regeneration of a large urban area, with increased green spaces, more sports infrastructure, and improved travel networks could be effective. This survey of young people and their parents found that although the regeneration from the Olympic Games did result in cleaner and safer environments, 18 months after the games well-being was not improved and there was no change in reported physical activity or sedentary behaviour between boroughs. It is likely that although the opportunity and infrastructure for sports and incidental physical activity were improved, other barriers to their use were not effectively addressed. Infrastructure is important, but further interventions to improve people’s motivation and capability to use the infrastructure may be important additional steps. Because this study relies on self-report about physical activity, it may not have captured important changes in the incidental physical activity generated through increases in walking in the improved urban environment or green spaces.
Ongoing research
Features of urban design that influence physical activity are being assessed by two ongoing projects. The ten Healthy New Towns across England are being evaluated for their success in improving the health of individuals and communities by applying healthy design principles to housing, transport, green spaces, waterways and community spaces. Identification of principles of healthy design, particularly as they encourage active leisure and transport, may guide urban development more widely (Study X). The ENABLE London (Study Y) project is examining how rapid changes to the local built environment following the Olympics can impact on health. In particular, the researchers are examining how the design of housing, roads, pavements, and outdoor spaces affect physical activity. A separate part of the project is also assessing whether the design of cities can reduce the risk of type 2 diabetes.
Active travel needs to be considered from a community point of view not a driver’s point of view. As the UK builds new housing communities, we need to think beyond connecting them with roads suitable only for cars.
Allison Coles, Research, Insight and Projects Manager, British Cycling
Adoption of 20 mph speed limits for traffic in residential areas is often justified in terms of improving perceived safety, and encouraging more walking and cycling. Such speed limits may also lead to more pleasant environments to live, work and play in. The ‘Is 20 plenty for health?’ study (Study Z) is assessing how effective these speed limits are, and exploring the differential impact on groups such as older people, parents, people with mobility difficulties, shift workers, and people from disadvantaged backgrounds.
The NIHR Public Health Research Programme is commissioning further research to understand the potential of place to have an impact on health and health inequalities, and research into choice architecture to assess how the presentation of everyday choices can influence people’s decision making and shape behaviours such as being more physically active.
Conclusions
This research has shown how, by redesigning our communities and environments to make physical activity an easy and attractive option, we can begin to move from a situation where inactivity is the default for many. Environments could be created that encourage a range of more active behaviours, particularly for people who are not already active. Reform of our transport systems, for example by providing free or cheaper public transport to reduce reliance on cars, may lead to a virtuous cycle of increasing people’s inclination to be active. Such reforms may reduce barriers such as traffic density which can frighten and discourage many from considering forms of active transport like walking or cycling, or from accessing opportunities for leisure. Policy-makers, strategists and planners are encouraged to set objectives in line with the NICE guidelines on physical activity and the environment (xxii) for the creation of physical activity friendly buildings, schools, streets and public spaces, so that even those who are least fit can confidently and safely use them for active travel and leisure.
Prompts for reflection
- What specific changes could improve the quality and appeal of local open spaces for those with low mobility, poor health, socioeconomic disadvantage, or specific cultural requirements?
- How are you able to increase physical activity through national and local coordination of changes to transport, planning, leisure, and health?
- What can you do to ensure the natural and built environment in ten or twenty years supports everyone to be physically active?
Discussion
This report highlights more than 50 published and ongoing studies funded by NIHR in the last few years to assess ways of getting people more active. This research addresses some important questions about what works best in getting particular groups of people active and helping them to stay active in the long term.
What can we learn from what worked?
Several initiatives to improve physical activity demonstrated real benefits. Many of these were designed using what we know of behavioural science and how people start and sustain good habits, as well as insight from participants. This included the programme delivered in football clubs for overweight men using peer support, coaching and goal-setting to achieve diet and activity changes, with participants staying active over time. Another study showed that breaking down activity goals into small, achievable changes and using pedometers, worked in getting adults and older people active and in maintaining their increased physical activity levels over the long-term. Other interventions, from standing desks at work to free bus travel, guided busways to increase walking and cycling to free access to leisure services, show the potential for real gains.
We know that there are no single solutions to the general problem of inactivity. How active we are depends on a number of complex and interconnected factors. This includes personal beliefs and habits and the wider demands and environment which shape how we live. This body of evidence shows the need for interventions to take account of what we know from the theory and practice of behaviour change. For example, as well as providing the right opportunities for physical activity, it is important to develop people’s motivations and capabilities to become more active. We also need to be realistic about the impact of short term single initiatives to improve activity levels, set against wider contexts and pressures.
Why do some promising interventions not work?
This research shows a mixed picture. Many promising evaluations of pilot initiatives did not result in increased activity when scaled up and tested in robust trials. This is true for a number of projects here, from dance classes for teenage girls to whole-school activity programmes in primary school. These high quality studies can give us more insights into why some of these plausible interventions may not have delivered the expected benefits. These include how children were approached to take part and the time and resources for teachers to deliver the intervention as planned. The large trial of a walking programme for those at high risk of diabetes did not show sustained activity levels in real-world settings, despite earlier positive findings. The reasons are complex but include poor attendance by those with poorest health status at start. Changes to the built environment in the Olympic park regeneration scheme did not deliver expected benefits. Improving the infrastructure is important but may not be enough on its own to change activity habits. On the other hand, the current state of the built environment and transport systems is generally so dissuasive of physical activity that it may effectively rule out positive results from physical activity interventions.
Some studies which did not show impact in terms of activity did deliver improvements in other ways, from reported well-being to reducing social isolation. We should not forget co-benefits of interventions. For instance, active transport schemes can help to reduce road traffic accidents, improve air or noise quality, and moderate climate change pressures, as well as potentially keeping people active. Policy makers are increasingly thinking now in terms of whole systems and joined-up planning, so that physical activity is not seen as an isolated goal, but an important aspect of many policies.
What do we still need to know?
Researchers are developing a better understanding of different types of intervention and how effective they can be, but many other opportunities to evaluate many projects and interventions are not taken. There are differences in general physical activity programmes for all and those which are targeted at particular groups of people. Factors such as income, employment, geography, gender, and ethnicity can all affect the chances of certain groups of people being active. Not everyone will have equal chances to take part in activities and many activities may just encourage those already active to do more, thus increasing inequalities. It is important that future research targets those with chronic levels of low activity and that we can evaluate tailored interventions to reach those who may benefit most. Learning from previous work, including the large-scale studies funded by Sport England provides useful insights, including the need to avoid using terms like ’sport’ and to re-frame activity in terms of social contact. There is a need for more research on activity which addresses the pressing inequalities agenda.
The studies here show how we can use opportunities which arise to measure impact and learn from new approaches. Several NIHR funded studies have used natural experiments to assess innovations as they occur, from Olympic Park regeneration to subsidised leisure to active transport measures, and have developed substantial expertise in these complex evaluations. To encourage more widespread evaluations of programmes, NIHR has launched phinder (xxiii) to match local innovations to research teams who can carry out evaluations as they happen. We want to hear about new initiatives which deserve robust evaluation so that others can learn from them.
NIHR and other research funders want to support more high quality research in this area, combining different disciplines ranging from physiology, public health, sports science to behavioural science. This is an exciting field bringing together different skills in a new way. There are opportunities for greater collaboration and consistency in approaches to physical activity research. These include how change is measured and how interventions are described. This should help to build up the knowledge base and capture learning more systematically, so that it can inform future implementation. Decision-makers need better understanding of quality evidence which is synthesised in a way which is clear but true to the science.
Given the declining levels of physical activity due to cultural, social and economic changes, and the capacity for physical activity to increase wellbeing and prevent many long term conditions, there is no room for complacency. To keep as well as possible, we need good evidence on getting more people active throughout their lives.
Appendices
Study summaries and references
Principal Investigator Kathryn Hesketh
(Funding: NIHR School for Public Health Research)
This international systematic review examined factors affecting physical activity change in young children. It included 44 quantitative studies with children aged 0-6. Two thirds of interventional studies were ‘multi-level’, targeting individual children, parents and teachers, whole organisations and/or the home environment. All the studies measured children’s change in physical activity behaviour, either objectively or subjectively. Outcomes included light, moderate and/or vigorous physical activity. Of 44 determinants of change, 14 were assessed in at least four papers. Of these, parental monitoring, involving logbooks and pedometers, showed a consistently positive association with change in child physical activity across intensities (four of six studies). Provider training was positively associated with change in moderate to vigorous physical activity (six of nine studies), but showed no clear association with physical activity overall. Five determinants (sex, parental goal setting, social support, motor skill training and increased time for physical activity) showed no clear association. The remaining seven (child knowledge, parental knowledge, parental motivation, parenting skills, parental self-efficacy, curriculum materials and portable equipment) were consistently not associated with change in children’s physical activity. Three further studies showed a positive effect of mothers as role models. Positive effects were often small in scale. The wide range of determinants and outcome measures used within the studies limited the authors’ conclusions.
Hesketh KR, O’Malley C, Paes VM, Moore H, Summerbell C, Ong KK et al. Determinants of change in physical activity in children 0–6 years of age: a systematic review of quantitative literature. Sports Medicine 2017 July;47(7): 1349–1374.
Study 2: Active for Life Year 5: A cluster randomised controlled trial of a primary school-based intervention to increase levels of physical activity, decrease sedentary behaviour and improve diet. 2016.
Principal Investigator Debbie A Lawlor
(Funding: NIHR PHR - 09/3005/04)
This trial investigated the effectiveness of a school-based intervention to increase children’s levels of physical activity, reduce sitting time and increase fruit and vegetable consumption. Participants were children from 60 English primary schools, aged 8-9 at recruitment (n= 2221). Half the schools received the intervention, delivered in Year 5. It included teacher training, 16 lesson plans and materials, ten parent-child homework assignments, and written materials for school newsletters. Primary outcome measures included accelerometer-assessed levels of physical activity and sedentary behaviour, and child-reported consumption of fruit and vegetables, assessed at Year 5-end, and a year later. The study found no difference in primary outcomes between children in intervention and control schools. The intervention appeared effective on three of nine secondary outcomes; children reported reducing weekend screen time by an average of 21 minutes per day, eating fewer snacks, and drinking fewer high-energy drink. Effects appeared to persist a year later, but differences might not have resulted from the intervention. The intervention cost to providers was approximately £18 per child. The researchers concluded that school-based interventions are unlikely to have a major impact on promoting physical activity and healthy diets in primary school children. They recommended research into more intensive family and community interventions.
Lawlor DA, Kipping RR, Anderson EL, Howe LD, Chittleborough CR, Moure-Fernandez A et al. Active for Life Year 5: a cluster randomised controlled trial of a primary school-based intervention to increase levels of physical activity, decrease sedentary behaviour and improve diet. Public Health Research 2016;4(7).
Principal Investigator Rob Anderson
(Funding: NIHR School for Public Health Research)
This systematic review examined the factors that lead to successful implementation of health promotion programmes in schools. The authors reviewed a wide range of international theoretical papers, from policy documents to qualitative research and systematic reviews. Twenty-two of these sources informed the development of a framework of what helps or hinders implementation. Evidence from 41 UK evaluation studies of school health promotion programmes was used to test the framework. These evaluations used a range of comparative designs, including randomised controlled trials and ‘before and after’ studies. Primary and secondary schools were included. The interventions included family smoking, education, sexual health education, a healthy lifestyle programme and various physical activities. The review found some in-depth evidence about how to prepare for implementation, and about initial implementation. This included the need for negotiation about programme delivery with staff and parents, addressing its acceptability to those who will deliver it, and highlighting short-term gains to both teachers and pupils. Evidence about embedding programmes into routine practice and adapting them for specific needs was more limited.
Pearson M, Chilton R, Wyatt K, Abraham C, Ford T, Woods HB et al. Implementing health promotion programmes in schools: a realist systematic review of research and experience in the United Kingdom. Implementation Science 2015;10:149
Principal Investigator Katrina Wyatt
(Funding: PHR - 10/3010/01)
This randomised controlled trial tested the effectiveness of a school-based healthy lifestyles programme in preventing obesity in children. Participants were 1324 children in Year 5 (aged 9-10 years) at recruitment, from 32 Devon primary schools, 14 of which had more than 19% of pupils eligible for free school meals. The programme comprised engaging with schools, children and families in the spring term of Year 5, a healthy lifestyles week with drama and goal-setting in the summer term, and reinforcement activities, such as promoting self-monitoring, early in Year 6. Half the schools received the intervention, half continued as usual. The main outcome measure was body mass index at 24 months after baseline (12 months post-intervention). Secondary outcomes included waist circumference, percentage body fat, accelerometer-assessed physical activity and food intake. A very high follow-up of 94% after two years was achieved. Results showed no difference in body mass index between children in the intervention and control schools at 24 months. There was no difference in secondary outcomes, apart from intervention children reporting consuming fewer unhealthy snacks and less unhealthy food generally. The cost of implementing the intervention was approximately £210 per child. The intervention successfully engaged children, families and teachers across the socioeconomic spectrum, but did not prevent overweight or obesity. The authors concluded that school-based programmes targeting one age group are unlikely to affect weight.
Wyatt K, Lloyd J, Creanor S, Green C, Dean SG, Hillsdon M et al. Cluster randomised controlled trial and economic and process evaluation to determine the effectiveness and cost effectiveness of a novel intervention [Healthy Lifestyles Programme (HeLP)] to prevent obesity in school children. Public Health Research 2018;6(1)
Principal Investigator Chris Bonell
(Funding: NIHR PHR - 09/3002/08)
This international review considered the effects of both primary and secondary school environments on student health, as distinct from curriculum-based health education. The main health topics included were violence, bullying, harassment, diet and physical activity. Three main aspects of the school environment were considered: management or school polices, catering services or vending machines, and sport or active transport. The researchers focused on schools’ organisation and management, teaching, pastoral care, discipline and physical environment, and analysed ten outcome evaluations in depth. Five examined interventions encouraging staff/students to build a stronger sense of community and/or better interpersonal relations. They generally reported benefits, such as to emotional health and aggression. Two evaluations assessed interventions modifying schools’ food/physical activity environments, and reported benefits for physical activity measures but not for diet. Three UK studies examined playground improvements and reported mixed findings on students’ physical activity. Process evaluations reported mainly positively on the feasibility and/or acceptability of interventions. Qualitative studies suggested that a lack of school safety, weak student/ staff relationships and lack of student participation in decisions may harm student health. The authors concluded that school environment interventions have the potential to promote student health, but the evidence is not clear-cut. They recommended conducting more trials that are welldesigned, and more research outside of the USA.
Bonell C, Jamal F, Harden A, Wells H, Parry W, Fletcher A. Systematic review of the effects of schools and school environment interventions on health: evidence mapping and synthesis. Public Health Research 2013;1(1)
Principal Investigator Ben Barr
(Funding: NIHR School for Public Health Research Public Health Practice Evaluation Scheme)
This study investigated whether providing children with free swimming access during school holidays increased their participation in swimming, and considered associations with neighbourhood deprivation. Children were aged 5-15, living in Blackpool. Blackpool Borough Council had been providing free swimming for under 16s during summer holidays since the national free swimming scheme for children ended in 2010. The comparator was a similar local authority which had ended its free swimming offer to children in 2010. The outcome was the number of children swimming, and the number of swim attendances, per 100 population in 2014. The study found similar rates of swimming for those aged 16 and over in Blackpool and in the comparison local authority. It found that free summer holiday swimming was associated with an extra 6% of children swimming, and an additional 33 swims per 100 children per year. The effects were greatest in areas of moderate deprivation, and smaller in the least and most deprived areas. Even so, an additional 4% of children from the most deprived areas participated in swimming. Study limitations included using areabased rather than individual indicators of socioeconomic status. The authors concluded that providing free access to swimming facilities to children living in a deprived local authority can increase their swimming participation and may help promote physical activity.
Higgerson J, Halliday E, Ortiz-Nunez A, Barr B. The impact of free access to swimming pools on children’s participation in swimming. A comparative regression discontinuity study. Journal of Public Health 2018; fdy079.
Lead Author Maureen Dobbins
(Funding: Cochrane Health Promotion and Public Health Field, Australia & City of Hamilton Public Health Services, Canada)
This international systematic review explored the effectiveness of school-based interventions in promoting physical activity and fitness in children and teenagers. It included 44 randomised controlled trials involving children aged 6-18 (n= 36,593). Interventions varied, and lasted from 12 weeks to six years. All focused on health promotion, were implemented mainly in a school-setting (sometimes also in the community and home), and included all pupils. Primary outcomes included rates of, and time engaged in, moderate to vigorous physical activity during the school day, and time spent watching television. Secondary outcomes included physical health measures. The authors found some evidence of positive effects of school curriculum changes, often with printed educational material. Time spent in physical activity increased by between five and 45 minutes per day across studies (mainly self-reported). Television time reduced by between five and 60 minutes per day (self/parentreported), and there were improvements in one physical health measure (maximal oxygen uptake). There was limited evidence of a positive effect on physical activity rates in children, but not in adolescents. The authors’ conclusions were limited by the studies’ risk of bias, and the generally small size of effects.
Dobbins M, Husson H, DeCorby K, LaRocca RL. Schoolbased physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database of Systematic Reviews 2013;2:CD007651.
Principal Investigator Russ Jago
(Funding: NIHR PHR - 11/3050/01)
This cluster randomised controlled trial investigated the effectiveness of a dance-based intervention in increasing girls’ physical activity levels. Participants were girls aged 11-12 (n= 571), in Year 7, in Bristol secondary schools. Girls opted to sign up following a ‘taster’ dance session offered to all. Experienced instructors delivered two free 75-minute dance sessions after school each week, for 20 weeks. Nine schools received the intervention; nine control schools continued as normal. The main outcome was accelerometer-assessed average minutes of weekday moderate to physical activity, one year after study start. Secondary outcomes included physical activity levels immediately after the intervention, and psychosocial outcomes. Results showed no differences between the intervention and control groups for physical activity at either time point. Only one third of girls in the intervention group attended at least two thirds of available dance sessions, although girls reported enjoying them. Attendance declined over time. The intervention cost an average of £73 per girl. Physical activity levels at baseline were high, suggesting the intervention appealed to already active girls. The authors noted the difficulty in maintaining attendance in secondary-school physical activity programmes, and the need for new ways to encourage adolescent girls to be physically active.
Jago R, Edwards MJ, Sebire SJ, Bird EL, Tomkinson K, Kesten JM, et al. Bristol Girls Dance Project: a cluster randomised controlled trial of an after-school dance programme to increase physical activity among 11- to 12-year-old girls. Public Health Research 2016;4(6)
Principal Investigator Judith Green
(Funding: NIHR PHR - 09/3001/13)
This study evaluated the health impacts of London’s free bus and tram travel policy for young people. It included secondary analysis of routine travel survey data and road accident records, interviews and focus groups, and literature reviews. Participants were young people aged 12-17 and older people aged at least 60, from two outer and two inner London boroughs. Changes in outcomes before and after the intervention were compared for young people, and adults aged 25-59 years (i.e. a population ineligible for the free travel policy). Results showed an increase in bus travel of almost a third over the period, for both adults and young people, especially for short journeys. Qualitative data suggested the policy had contributed to bus travel becoming the ‘default’ mode for many journeys. There was no significant overall reduction in walking, but no evidence of a beneficial effect on physical exercise. There was a reduction in road traffic injuries for car occupants and cyclists, consistent with the reduction in car occupancy and cycling, but which may have been due to other interventions over the period. There was no evidence of an adverse impact on travel for older people. Interviews suggested a positive effect on young people’s well-being, including on sociability and feelings of belonging.
Green J, Steinbach R, Jones A, Edwards P, Kelly C, Nellthorp J et al. On the Buses: A mixed method evaluation of the impact of free bus travel for young people on the public health. Public Health Research 2014;2(1)
Principal Investigator Melanie J Davies
(Funding: NIHR PHR - 13/90/30)
This trial explored the effectiveness of the Girls Active intervention. It was a two-arm cluster randomised controlled trial, with interviews and focus groups alongside. Participants (n=1752) were girls aged between 11 and 14 years attending 20 state secondary schools in the Midlands, UK. At least 80 girls were randomly selected to take part from each school (around 30 from each year group). The intervention provides a support framework for schools to review and change their physical activity, physical education and school sport culture and practices. Lead teachers attend training, review their schools and create action plans. They identify and work with girls to become peer leaders, encouraging other girls to be more active. Half the schools received the intervention, half carried on with usual practice. The main outcome was change in accelerometer-measured moderate to vigorous physical activity level at 14 months, (available for 69% of participants). Results showed no overall impact of the intervention on physical activity levels at 14 months. Teachers and girls who became peer leaders viewed the intervention positively, but some pupils reported they had not fully understood it. Workload meant teachers did not implement everything they wanted to. The per pupil intervention cost ranged by school from £23 to £95.
Harrington DM, Davies MJ, Bodicoat D, Charles JM, Chudasama YV, Gorely T et al. A school-based intervention (‘Girls Active’) to increase physical activity levels among 11- to 14-year-old girls: cluster RCT. Public Health Research 2019;7(5)
Principal Investigator Chris Power
(Funding: Department of Health Policy Research Programme through the Public Health Research Consortium and supported by the NIHR Biomedical Research Centre at Great Ormond Street Hospital for Children NHS Foundation Trust and University College London.)
This study analysed influences from early adulthood on patterns of midlife leisure-time inactivity. It used information from participants of the 1958 British Birth Cohort who were living in Britain aged 50. Early adult factors, recorded at 23 and 33 years, included physical status, depression, education level, social, family and neighbourhood circumstances. The outcome was selfreported inactivity at 33 or 50 years (n=12,271). Leisuretime inactivity was defined as participating less than once a week in regular activity of mostly moderate or vigorous intensity, such as swimming or going for walks. The study found that between the ages 33-50 years, 51% of respondents were never inactive, 14% were persistently inactive and 35% changed their inactivity status (17% deteriorated to inactivity and 18% improved from inactivity). Two factors from young adulthood – obesity and neighbourhood lived in – had long-lasting associations with midlife inactivity patterns. Compared to those who were not obese at either 23 or 33 years, those who were obese at both ages had higher odds of persistent inactivity (74%) and inactivity deterioration (56%), and 38% lower odds of improvement. Compared to those living in suburbs, service centres, rural areas or seaside resorts, living in industrial / local authority housing areas was associated with higher odds of inactivity persistence (59%) and deterioration (30%), and 25% lower odds of improvement. The authors noted these findings can help identify groups likely to benefit from inactivity interventions, and highlight how, via inactivity, neighbourhood can potentially influence future health.
Pinto Pereira SM and Power C. Early adulthood determinants of mid-life leisure-time physical inactivity stability and change: Findings from a prospective birth cohort. Journal of Science and Medicine in Sport 2018 July;21(7):720-726. Published online 22 November 2017.
Principal Investigator Cindy M Gray
(Funding: NIHR PHR - 13/99/32)
This study investigated long-term outcomes of the Football Fans in Training programme. Participants were overweight or obese men aged 35-65, who had taken part in a 2011/12 trial (n=665), or later participated in a routinely delivered programme (n=511). The intervention comprised 12 free weekly group-based advice and physical activity sessions, delivered by coaches at professional Scottish football clubs. Sessions include dietary advice, self-monitoring, goal-setting and feedback, and coach-led physical activity. Mutual learning and support are encouraged. The trial group were compared with the routine delivery group. The primary outcome was long-term weight loss after 3.5 years.Trial intervention participants still weighed an average of 2.9kg less. Almost a third had kept off at least 5% of their starting weight, but around two thirds had not. Participants showed long-term improvements in body mass index, waist circumference, percentage body fat, blood pressure, selfreported physical activity, diet, self-esteem and well-being. At 3.5 years, men reported walking an extra 90 minutes per week more than at baseline. Routine programme participants showed similar long-term benefits, suggesting its effectiveness beyond research conditions. Men continued to self-monitor weight, physical activity and diet, and to engage with other participants and coaches. The authors recommended further research into achieving greater weight loss outcomes through the programme.
Gray CM, Wyke S, Zhang R, Anderson AS, Barry S, Brennan G, et al. Long-term weight loss following a randomised controlled trial of a weight management programme for men delivered through professional football clubs: the Football Fans in Training follow-up study. Public Health Research 2018;6(9)
Study 13: Walking Away from Type 2 diabetes: a cluster randomized controlled trial. 2017
Principal Investigator Tom Yates
(Funding: NIHR CLAHRC for Leicestershire, Northamptonshire and Rutland & NIHR CLAHRC – East Midlands)
This trial investigated an intervention to promote and sustain increased walking activity. Participants (n=808) were from 10 general practices, scored highly on a Type 2 diabetes risk score, aged 18-74, and 36% female. Half the practices received the intervention, comprising a threehour group-based education session, goal setting, selfmonitoring via pedometer, annual refresher sessions, and brief telephone support. Control participants received an information booklet. The main outcome was accelerometerassessed steps/day at 12 months, and also at 24 and 36 months. Results found an increase of 411 steps/day at 12 months in the intervention group, compared with the control. Differences were not maintained at 36 months. The authors noted their pilot study had found a much larger effect of 2000 steps/day over 12 months, illustrating the difficulties of implementing physical activity interventions in routine primary care settings. They concluded that, since those with raised glucose levels at baseline appeared more successful in changing their behaviour at 12 months, testing glucose levels at the outset may help motivate people and improve success. Furthermore, 23% of intervention participants did not attend the initial group session, and tended to have worse health status indicators than those who did attend, suggesting more personalised approaches may help. A follow-on study will investigate further.
Yates T, Edwardson CL, Henson J, Gray LJ, Ashra NB, Troughton J et al. Walking Away from Type 2 diabetes: a cluster randomized controlled trial. Diabetic Medicine 2017;34(5):698-707. First published 02 September 2016.
Principal Investigator Fiona Campbell
(Funding: NIHR HTA - 13/45/01)
This review analysed the effectiveness of exercise referral schemes, in which health professionals refer patients to external exercise providers to increase their physical activity levels. It combined data from eight randomised controlled trials (n= 5190 adult participants) and from linked qualitative studies. Interventions involved in-person or telephone counselling, written materials, or supervised exercise training, for varying lengths of time. Comparators were: no intervention or brief advice (n=5), motivational counselling (n=1) or alternative schemes (n=2). The most common outcome was self-reported physical activity. The authors concluded that exercise referral schemes result in a small increase in self-reported physical activity. Referral did not lead to changes in objective measures of health such as weight or blood pressure. People without their own transport, or living in more deprived neighbourhoods, were less likely to take up a referral. People with a history of being more physically active, who received a referral due to their risk of coronary heart disease, or who were older, were more likely to increase their physical activity levels. The authors’ recommendations for future research included investigating which groups benefit more from the schemes, which aspects are most effective, and comparisons with a non-exercise intervention with a potential social benefit (such as choirs).
Campbell F, Holmes M, Everson-Hock E, Davis S, Buckley Woods H, Anokye N, et al. A systematic review and economic evaluation of exercise referral schemes in primary care: A short report. Health Technology Assessment 2015;19(60)
Principal Investigator Tess Harris
(Funding: NIHR HTA - 10/32/02)
This randomised controlled trial assessed the effectiveness, cost-effectiveness and acceptability of a pedometer-based walking intervention. The intervention used behaviour change techniques. The trial included 1,023 inactive adults (10% of those approached), aged 45 to 75, from London general practices. They were assigned, by household, to usual care, postal intervention, or nurse-support intervention. The postal group received a pedometer, diary and 12-week walking programme, advising them to gradually add ‘3000 steps in 30 minutes’ at least five days weekly. The nurse-support group received the same materials with three practice nurse consultations. The main outcomes, measured with accelerometers, were changes over 12 months in average daily step counts, and time in moderate to vigorous physical activity levels. Ninety three percent of participants provided outcome data at 12 months. On average, both interventions increased 12-month step counts by around one-tenth (660 extra steps per day), and time in moderate to vigorous physical activity by around one-third (34 extra minutes per week). The benefits persisted for at least three years. There were no differences in physical activity outcomes between the postal and nurse-supported groups, but the postal route was more cost-effective in both the short and long-term. Qualitative evaluations indicated that participants and nurses found the interventions acceptable and enjoyable. The authors suggested adopting ‘3000 steps in 30 minutes’ as a public health goal, and researching the integration of the 12-week programme into commonly used wearable devices.
Harris T, Kerry S, Victor C, Iliffe S, Ussher M, Fox-Rushby J, et al. A pedometer-based walking intervention in 45- to 75-year-olds, with and without practice nurse support: the PACE-UP three-arm cluster RCT. Health Technology Assessment 2018;22(37)
Principal Investigator Louise Lafortune
(Funding: National Institute for Health and Care Excellence (NICE) & NIHR School for Public Health Research)
This systematic review examined barriers and facilitators to people at mid-life undertaking and maintaining healthy behaviours. It reviewed international evidence from 46 systematic reviews (19 focused on physical activity), 28 qualitative studies and 11 longitudinal cohort studies. The review included studies targeting adults in mid-life (40 to 64 years) and younger adults in disadvantaged or minority groups who are at higher risk of health inequalities. It identified evidence relating to the uptake and maintenance of physical activity, diet and nutrition, weight loss, smoking, alcohol, eye care and other health promoting behaviours. It excluded studies about participation in, or effectiveness of, specific interventions. Evidence quality ranged from low to high. Barriers to physical activity participation included existing physical ill-health, lack of time, neighbourhood safety, financial cost, lack of availability/access, lack of motivation, low self-belief and low socioeconomic status. Facilitators included focusing on improved wellbeing and self-esteem, health benefits in general, promoting healthy ageing, enjoyment of the activity, integrating physical activity into everyday life, focusing on short-term benefits, being a good role model and being supported by others. The authors concluded that this information could help tailor health interventions for people in mid-life.
Kelly S, Martin S, Kuhn I, Cowan A, Brayne C, Lafortune L. Barriers and Facilitators to the Uptake and Maintenance of Healthy Behaviours by People at Mid-Life: A Rapid Systematic Review. PLoS ONE 2016;11(1): e0145074.
Principal Investigator Emma Solomon-Moore
(Funding: NIHR CLAHRC & South West Peninsula and Economic and Social Research Council)
This trial evaluated whether a community-level physical activity intervention increased the activity levels of rural communities. 128 rural villages were randomly allocated to receive the intervention in one of four time periods from April 2011-December 2012, until all had received it. A postal survey was sent to samples of adults within the villages before study start, and following each intervention period; 10,412 adults completed the survey in total across these five data collection phases (response rate 32%). The intervention comprised 12 weeks of physical activity for all ages, with at least three subsidised activities and 12 months’ follow-up support. Before the intervention, delivery partners (including district authorities and charities) surveyed local people about their preferred activities. Activities were then tailored to each village and included children’s basketball, multi-sports sessions for adolescents and adult fitness classes. The main outcome was adults’ self-reported physical activity levels. Minutes spent in moderate-and-vigorous activity per week was a secondary outcome. Only 16% of participants reported awareness of the intervention programme, and just 4% participated in the activities. The intervention did not increase the chances of adults meeting the physical activity guideline, but there was weak evidence of an increase in minutes of moderate-and-vigorous activity. The authors concluded that the intervention’s ineffectiveness might have been due to its low uptake, and that future research could investigate achieving greater community engagement.
Solomon E, Rees T, Ukoumunne OC, Metcalf B and Hillsdon M. The Devon Active Villages Evaluation (DAVE) trial of a community-level physical activity intervention in rural south-west England: a stepped wedge cluster randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2014;11:94
Principal Investigator Ben Barr
(Funding: NIHR School for Public Health Research Public Health Practice Evaluation Scheme)
This study investigated the effect of removing charges from gyms and leisure centres on overall levels of physical activity. It analysed attendance data from nine leisure centres in Blackburn with Darwen, from 2005-2014, and used the Active People Survey to compare changes in physical activity in Blackburn with Darwen after the intervention, to change in national comparator areas. The re:fresh intervention,introduced in 2008, provided free access to swimming pools and gyms for people aged 16 and over. Free leisure was available to the whole population for 90% of the facilities’ opening hours overall. It included marketing, community engagement sessions, and individual and group behaviour change sessions for around 700 inactive people per year, delivered by five health trainers. Outcomes included attendance at swimming and gym sessions, and self-reported participation in gym, swim and any physical activity. Results found free leisure was associated with a 64% increase in attendances at swimming and gym sessions, and an extra 4% of local people participating in at least 30 minutes of moderate-intensity gym or swim sessions during the previous four weeks. An extra 2% of the population participated in any sport or active recreation of at least moderate intensity for at least 30 minutes on at least 12 days out of the last four weeks. These effects were significantly greater for the more disadvantaged socioeconomic group. The authors concluded with outreach and marketing activities, can increase overall population levels of physical activity while reducing inequalities.
Higgerson J, Halliday E, Ortiz-Nunez A, Brown R, Barr B. Impact of free access to leisure facilities and community outreach on inequalities in physical activity: a quasie-xperimental study. Journal of Epidemiology & Community Health 2018;72:252-258.
Principal Investigator Ruth Garside
(Funding: NIHR School for Public Health Research)
This study assessed the health and well-being impacts on adults who participated in environment and conservation activities. It systematically reviewed international quantitative and qualitative evidence. Participants were adult volunteers, or referred by a healthcare professional. The researchers identified 211 grey literature records and included 19 studies in their synthesis (n=3648 total participants): seven quantitative, nine qualitative, and three mixed methods. Most studies were internal programme evaluations, and most had fewer than 100 participants. There was no randomised controlled evidence. Activities included tree planting, making pathways and woodland management. Most of the quantitative studies found no effect on health and well-being. There was limited and mixed evidence of positive impacts on self-reported health and physical activity, and negative impacts including increased anxiety. Qualitative evidence suggested that participants enjoyed the social contact, especially if they were isolated or experiencing mental ill-health, and other positive experiences included feeling a sense of achievement, being outside and having a structured day. The researchers noted that the research was mainly of low quality, both in design and reporting, so they could not draw definitive conclusions. Future, more robust, research should investigate the effects of these activities, and their potential role in health promotion.
Husk K, Lovell R, Cooper C, Stahl-Timmins W, Garside R. Participation in environmental enhancement and conservation activities for health and well-being in adults: a review of quantitative and qualitative evidence. Cochrane Database of Systematic Reviews 2016; 5:CD010351.
Study 20: Modifying health promotion interventions to meet the needs of ethnic minority groups. 2012
Principal Investigator Aziz Sheikh
(Funding: NIHR HTA - 07/63/03)
This study considered the appropriateness and effectiveness of health promotion interventions for smoking cessation, increasing physical activity and improving healthy eating, for African-, Chinese- and South Asian-origin populations. It comprised launch and end-of-study conferences, analysis of guidelines and systematic reviews, a systematic review of adapted interventions, and interviews with researchers and health promoters. The authors identified 15 relevant UK guidelines and 111 international systematic reviews. Their search extended to community and wider interventions, but most research focused on individual-centred behavioural approaches. Overall evidence for physical activity and healthy-eating interventions in the general population was limited. The most consistent evidence of effectiveness was for medication for smoking cessation, but there was little evidence about ethnic minority populations. The authors reviewed 173 reports of adapted health promotion interventions, which informed their practical adaptation framework. Most studies focused on US-based African Americans. Only nine studies directly compared the effectiveness of culturally adapted with standard interventions, and evidence was inconsistent. Twenty-six interviews with researchers, and those delivering adapted health promotions, emphasised the need to consider contextual issues. The authors concluded that adapting interventions for ethnic minority communities should be considered. More research is required comparing standard and culturally adapted interventions, including UK-based studies.
Liu JJ, Davidson E, Bhopal R, White M, Johnson MRD, Netto G, Deverill M, Sheikh A. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis. Health Technology Assessment 2012;16(44)
Study 21: Workplace interventions for reducing sitting at work. 2018
Lead Author Nipin Shrestha
(Funding: Cochrane Work Review Group, NIHR CLAHRC West & Victoria university, Australia)
This systematic review explored the effectiveness of workplace interventions to reduce sitting at work. It included 34 studies, of which 26 were randomised controlled trials, and eight were controlled before-and-after studies. Participants (n= 3,397 in total) were employees from highincome countries. Interventions included physical workplace changes, workplace policy changes, information and counselling and multi-part interventions. Interventions were compared to no intervention or alternative interventions. The primary outcome was self-reported or objectively-measured time spent sitting at work per day. The authors found low quality evidence that sit-stand desks, either alone or combined with information and counselling, reduced sitting time at work compared to sit-desks. The average reduction was by 100 minutes per workday at up to three months follow-up, and by 57 minutes per day at 3-12 months follow-up. The effects of other interventions such as ‘active workstations’ (treadmill or cycling desks), walking during breaks, and information and counselling, were mostly inconsistent or there was insufficient evidence to draw conclusions. The authors found the quality of evidence was low to very low for most interventions. They concluded that larger trials with longer-term follow-up were needed.
Shrestha N, Kukkonen-Harjula KT, Verbeek JH, Ijaz S, Hermans V, Pedisic Z. Workplace interventions for reducing sitting at work. Cochrane Database of Systematic Reviews 2018;12:CD010912.
Principal Investigators Fehmidah Munir and Charlotte L Edwardson
(Funding: Loughborough University, Department of Health Policy Research Programme & NIHR Leicester Biomedical Research Centre)
This randomised controlled trial tested an intervention to reduce sitting time at work, building on an earlier Cochrane review (Shrestha, 2018). Participants (n=146) worked in 37 office groups within three NHS hospitals. The intervention included a group education session about the health consequences of sitting; a personalised action plan; provision of a sit-stand workstation; a sitting self-monitoring and prompt device; feedback on sitting and physical activity three times; and one-to-one brief coaching every three months. Intervention groups were compared with usual practice groups. The main outcome was accelerometer-measured sitting time at work. Secondary outcomes included daily sitting, standing time, physical activity, musculoskeletal problems and self-reported work-related and psychological health. Outcomes were assessed at three, six and twelve months. The intervention group showed reduced sitting at each time-point in comparison to the control group. The largest difference was at 12 months, when intervention participants were sitting at work for an average of 83 minutes less each day and standing more than the control group. There was no difference between groups in daily moderateto- vigorous activity or daily stepping time. The intervention group showed some improvement in work related and psychological health. A larger, longer-term trial is now testing the intervention further.
Edwardson CL, Yates T, Biddle SJH, Davies MJ, Dunstan DW, Esliger DW et al. Effectiveness of the Stand More AT (SMArT) Work intervention: cluster randomised controlled trial. BMJ 2018;363:k3870.
Principal Investigator Frank Kee
(Funding: NIHR PHR-12/211/82)
This trial evaluated the effectiveness of a loyalty scheme for increasing physical activity. Participants (n= 853) were healthy employees, aged 18-65, in nine public sector organisations in Northern Ireland. The loyalty card scheme enabled participants to earn points for minutes of physical activity, which converted into local retail vouchers. Sensors were placed within a 2 km radius of workplaces, and logged participants’ physical activity via keyfobs. Participants set goals and monitored themselves, and received personalised motivational emails, feedback and information. A waiting-list control group were able to participate following trial completion. The main outcome was pedometer-measured average steps per day after six months, also collected at 12 months. (54% of intervention and 60% of control participants provided data.) Secondary outcomes included self-reported workplace physical activity, health and wellbeing. Results found a significant reduction in average steps/day in the intervention group at 6 months, and no difference between groups at 12 months. Secondary outcomes were inconsistent; higher mental wellbeing scores for intervention participants were not matched by findings from the quality of life and mental health measures. The authors noted that early technological problems caused frustration, and significant organisational re-structuring may have limited the intervention. The trial highlighted implementation challenges.
Hunter RF, Murray JM, Gough A, Tang J, Patterson CC, French DP et al. Effectiveness and cost-effectiveness of a loyalty scheme for physical activity behaviour change maintenance: results from a cluster randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2018;15:127.
This systematic review assessed international evidence about the types, effectiveness and acceptability of interventions to increase physical activity in people around retirement age. Only one study specifically examined the transition to retirement, highlighting a clear evidence gap. The researchers broadened the search and examined 103 effectiveness studies in adults (mainly women) aged 49-75, alongside 55 qualitative papers. Interventions included training of healthcare professionals; counselling and advice giving; group and individual sessions; in-home programmes; and communitywide initiatives. Most studies compared several interventions. They measured a range of outcomes, reflecting inconsistency in the aims of physical activity interventions. Outcomes were mostly self-reported and included activity levels, fitness levels and psychosocial elements. Only two studies assessed sedentary behaviour. Most studies reported positive outcomes. Although older adults felt that enjoyment and socialising were important aspects of activity programmes, few interventions focused on this. Given the lack of evidence, the authors could not recommend specific interventions for people of retirement age, but concluded that a range of interventions may be effective, including group and individual sessions. Including a social element, being free or low cost, and meeting individual preferences, may increase the effectiveness of interventions. Future studies should evaluate effectiveness using robust, objective measures.
Baxter S, Blank L, Johnson M, Everson-Hock E, Woods HB, Goyder E, et al. Interventions to promote or maintain physical activity during and after the transition to retirement: an evidence synthesis. Public Health Research 2016;4(4)
Principal Investigator Louise Lafortune
(Funding: NIHR School for Public Health Research & CLAHRC - East of England)
This review of 40 international systematic reviews explored the effectiveness of physical activity for prevention of cognitive decline (n=14 reviews), interventions to increase and maintain physical activity levels (n=17 reviews), and barriers and facilitators to physical activity (n=9 reviews), for people aged over 55. The quality of evidence ranged from low to high. Interventions varied widely; details of intensity or duration were missing in half the reviews. No reviews reported outcomes of reduced incidence of dementia; outcomes related to short-term improvement in cognitive function. The authors found small positive effects of physical exercise on cognition amongst older people with normal cognition or mild cognitive impairment, but no conclusive evidence about the best type of exercise. A variety of interventions were effective for increasing older people’s short-term uptake of physical activity, including behavioural (walking and exercise) and cognitive (education and motivational interviewing). Few studies included long-term follow-up. Barriers to older people’s uptake and maintenance of physical activity included: health status, previous habits and experiences, low self-belief, time, access, cost, and environmental safety. Facilitators included: enjoyment, personal challenge, support, communication, information, access and convenience. Recommendations for future research included exploring the duration and intensity of physical activity required to produce effects, and long-term maintenance of physical activity.
Olanrewaju O, Kelly S, Cowan A, Brayne C, Lafortune L. Physical Activity in Community Dwelling Older People: A Systematic Review of Reviews of Interventions and Context. PLoS ONE 2016;11(12):e0168614.
Principal Investigator Steve Iliffe
(Funding: NIHR HTA - 06/36/04)
This trial compared a class-based and a home-based exercise programme with usual care. Participants were aged 65 or over (n=1256), from 43 general practices. The home-based programme involved 30 minutes of leg strengthening and balance exercises at least three times weekly, and encouraged two 30-minute walks per week. Peer mentors, where available, provided up to five home visits and 12 telephone contacts. The community class-based programme comprised weekly hour-long classes with a postural stability instructor, plus two 30-minute home exercise sessions, and encouraged two 30-minute walks per week. Both interventions lasted for 24 weeks. The primary outcome was self-reported physical activity 12 months after programme-end. Secondary outcomes included balance confidence, number of falls, and quality of life. Results showed an absolute increase of 14% more participants in the class-based exercise group reached the recommended level of 150 minutes of moderate to vigorous physical activity per week, compared to those receiving usual care. Participants added 13-15 minutes per day to their baseline physical activity level. The classbased group also experienced a reduction in falls. Both intervention groups showed improved balance confidence, but otherwise the home-based exercise group showed no significant difference to those experiencing usual care. Neither intervention made a significant difference to quality of life. The class-based programme cost £269 per participant in London (£218 in Nottingham).
Iliffe S, Kendrick D, Morris R, Masud T, Gage H, Skelton D et al. Multi-centre cluster randomised trial comparing a community group exercise programme with home based exercise with usual care for people aged 65 and over in primary care. Health Technology Assessment 2014;18(49)
Principal Investigator Denise Kendrick
(Funding: NIHR School for Primary Care Research)
This cohort study examined factors associated with maintaining physical activity after completing an exercise programme within the trial described in Study 26. Participants were aged 65 or over, had received the classbased intervention, home-based intervention or usual care, and provided follow-up physical activity data at least once (n=731). Participants were mainly female, white, with a high level of education and higher socio-economic status, limiting the generalisability of the findings. After the interventions, participants received information about local exercise opportunities. Self-reported moderate to vigorous physical activity levels, and factors potentially associated with physical activity, were recorded at recruitment, 6, 12, 18 and 24 months after the exercise programme. The authors found that older people and women were less likely to achieve target physical activity levels. Those already physically active when recruited, with greater lower limb strength, and with wider social networks, were more likely to achieve the target. These effects persisted across the follow-up period. The strongest association with physical activity maintenance was physical activity at recruitment. The authors recommended that maintenance programmes should target those least likely to maintain physical activity, including older women, those with narrower social networks and those with poorer lower limb strength.
Kendrick D, Orton E, Lafond N, Audsley S, Maula A, Morris R et al. Keeping active: maintenance of physical activity after exercise programmes for older adults. Public Health 2018 Nov;164:118-127.
Study 28: Health impacts of the Cambridgeshire Guided Busway: a natural experimental study. 2016
Principal Investigator David Ogilvie
(Funding: NIHR PHR - 09/3001/06)
This study assessed how a new bus network and pedestrian/cycle path affected people’s travel to work, and associated impacts on health. Researchers analysed a cohort of users from 2009 (n=1143) to 2012 (n=470), conducting annual surveys and detailed quantitative studies of activity patterns using travel diaries, accelerometers, body sensors and global positioning system receivers. They surveyed busway users (n= 1710), and conducted over 120 semi-structured interviews with cohort and survey participants. Cohort participants were adults living within 30km of Cambridge city centre and working in the city. The busway opened in 2011, comprising 22km of dedicated bus lane plus an off-road path for pedestrians and cyclists. Researchers compared participants by distance lived from the busway. The main outcome was time spent in active commuting (self-reported and objectively confirmed). Many factors affected commuting decisions, including childcare and parking. People often combined walking and cycling with longer bus or car journeys. Overall, those living closer to the busway were more likely to have increased their active commuting time, reduced the number of car-only trips, and increased their weekly cycle commuting time. Those who spent more time actively commuting were more likely to show higher accelerometer-recorded levels of overall physical activity, and report higher levels of physical well-being.
Ogilvie D, Panter J, Guell C, Jones A, Mackett R, Griffin S. Health impacts of the Cambridgeshire Guided Busway: a natural experimental study. Public Health Research 2016;4(1)
Principal Investigator David Ogilvie
(Funding: NIHR PHR - 11/3005/07)
This study assessed the health effects of a new urban motorway on local communities. The study repeatedly surveyed adults recruited in 2005 (n=1345) and 2013 (n=1343). Of these, 365 participants provided data at baseline and follow-up. 196 survey participants used accelerometers and global positioning system receivers to measure physical activity. Researchers conducted interviews and analysed national road traffic accident and travel behaviour data. Motorway intervention area participants were compared with those in two matched control areas: one near an existing motorway, and one with no major road infrastructure. The main outcome measures were differences in self-reported travel behaviour, physical activity and well-being, and in the number of road traffic accidents. The researchers identified both benefits and harms. People living closer to the new motorway experienced significantly reduced mental well-being over time compared with those living further away. There was an increase in travel generally (particularly car use), no overall change in active travel or accidents, and weak evidence of reduced physical activity participation. Qualitative evidence suggested the new motorway helped connect people with dispersed social networks and car access, but cut off others from local people and places. The researchers concluded that large urban infrastructure projects can increase inequalities and reduce health outcomes in already disadvantaged communities.
Ogilvie D, Foley L, Nimegeer A, Olsen JR, Mitchell R, Thomson H, et al. Health impacts of the M74 urban motorway extension: a mixed-method natural experimental study. Public Health Research 2017;5(3).
Principal Investigator Steven Cummins
(Funding: NIHR PHR - 09/3005/09)
This study assessed how the London 2012 Olympic and Paralympic Games affected the physical activity and mental health and well-being of local residents. Participants were adolescents (n=2254) aged 11-12 years at baseline, and a sample of their parents/carers. The Olympic Park was redeveloped for ongoing public use. Residents in the intervention area were compared with those living in nearby Boroughs but not receiving urban regeneration on the same scale. The main outcome measures were change in self-reported physical activity, self-reported depression and anxiety, and well-being score. Data were collected before the intervention and at six and 18 months afterwards. At six months, adolescents who became inactive were less likely to come from the intervention borough. At 18 months, there were no significant differences between intervention and comparison boroughs for all adolescent physical activity. No impacts on parent/carer physical activity were observed. Over time, people’s mental health or well-being did not improve. Interviews found that residents generally welcomed their cleaner, safer and more ‘unified’ living environment. The authors concluded that the Games generated a sense of social inclusion and relief from everyday stressors, even if only temporarily. The most strongly expressed local need was for housing, which was not part of the intervention. Limitations included reductions in central and local public spending at the time.
Cummins S, Clark C, Lewis D, Smith N, Thompson C, Smuk M et al. The effects of the London 2012 Olympics and related urban regeneration on physical and mental health: the ORiEL mixed-methods evaluation of a natural experiment. Public Health Research 2018;6(12)
Ongoing and feasibility studies
Study A: Startwell: a service evaluation of nutritional and physical activity training for early years staff
Principal Investigator or Lead Author: Kate Jolly
Study B: NAP SACC UK: A feasibility cluster randomised controlled trial in child care settings to increase physical activity and healthy eating in 2-4 year olds
Principal Investigator or Lead Author: Ruth Kipping
Study C: CLASS PAL Study
Principal Investigator or Lead Author: Lauren Sherar
Study D: The impact of a family-based physical activity promotion programme on child physical activity: feasibility and pilot of the Families Reporting Every Step to Health (FRESH) intervention
Principal Investigator or Lead Author: Esther Van Sluijs
https://www.journalslibrary.nihr.ac.uk/programmes/phr/150119#/
Study E: Stand Out in Class: Restructuring the classroom environment to reduce sedentary behaviour - a pilot cluster randomised controlled trial
Principal Investigator or Lead Author: Stacey Clemes
Study F: Action 3:30: A cluster randomised feasibility study evaluation of a teaching assistant led, extracurricular physical activity intervention for 8 to 10 year olds
Principal Investigator or Lead Author: Russ Jago
Study G: Engaging adolescents in changing behaviour (EACh-B): a programme of research to improve the diets and physical activity levels of teenagers
Principal Investigator or Lead Author: Mary Barker
Study H: Understanding the sustainable processes and impact of engaging young people in a peer-led dance group, the TR14ers
Principal Investigator or Lead Author: Katrina Wyatt
Study I: A cluster randomised controlled trial to evaluate the effectiveness and cost-effectiveness of the GoActive programme to increase physical activity among 13-14 year-old adolescents
Principal Investigator or Lead Author: Kirsten Corder
Study J: A cluster randomised controlled trial of a Peer-Led physical Activity iNtervention for Adolescent girls (PLAN-A)
Principal Investigator or Lead Author: Russ Jago
Study K: The Yoga Study
Principal Investigator or Lead Author: Tom Yates
Study L: Delivering a realistic Diabetes Prevention Programme in a UK community
Principal Investigator or Lead Author: Mike Sampson
Study M: Active buildings: modelling physical activity and movement in office buildings. An observational study protocol
Principal Investigator or Lead Author: Lee Smith
Study N: Impact of sit-stand desks at work on energy expenditure, sitting time and cardio-metabolic risk factors: Multiphase feasibility study with randomised controlled component
Principal Investigator or Lead Author: Eleni Mantzari
Study O: UP FOR 5
Principal Investigator or Lead Author: Charlotte Edwardson
Study P: Stand Up For Health: A Feasibility Cluster Randomised Controlled Trial (RCT) Of A Theory Based Intervention To Reduce Sedentary Behaviour In Contact Centres
Principal Investigator or Lead Author: Ruth Jepson
Study Q: A three arm cluster randomised controlled trial to test the effectiveness and cost-effectiveness of the SMART Work & Life intervention for reducing daily sitting time in office workers
Principal Investigator or Lead Author: Charlotte Edwardson
Study R: The effectiveness and cost effectiveness of an employer-led intervention to increase walking during the daily commute: Cluster randomised controlled trial
Principal Investigator or Lead Author: Suzanne Audrey
Study S: A cluster randomised controlled trial to investigate the effectiveness and cost-effectiveness of a Structured Health Intervention For Truckers (The SHIFT Study)
Principal Investigator or Lead Author: Stacey Clemes
Study T: A randomised controlled trial and economic evaluation of a communitybased physical activity intervention to prevent mobility-related disability for retired older people. The REACT (REtirement in ACTion) study
Principal Investigator or Lead Author: Afroditi Stathi
Study U: A feasibility study and pilot RCT of a peer-led walking programme to increase physical activity in inactive older adults: Walk With Me Study
Principal Investigator or Lead Author: Mark Tully
Study V: Chair based exercise in community settings: a cluster randomised feasibility study
Principal Investigator or Lead Author: Tahir Masud
Study W: A pilot study of a peer volunteering intervention for promoting active ageing in the community: Project ACE
Principal Investigator or Lead Author: Selena Gray
Study X: The long-term health and wellbeing impacts of Healthy New Towns: a six-month feasibility study of Healthy New Town demonstrator sites in England
Principal Investigator or Lead Author: Angela Harden
Study Y: Does active design increase walking and cycling? Evaluation of a natural experiment examining whether moving into housing in East Village increases family levels of physical activity, particularly walking and cycling.
Principal Investigator or Lead Author: Christopher Owen
Investigating how the design of cities can reduce the risk of type 2 diabetes
Principal Investigator or Lead Author: Christopher Owen
Study Z: Is 20 plenty for health? Evaluation of the 20mph speed limit networks in Edinburgh and Belfast on a range of public health outcomes
Principal Investigator or Lead Author: Ruth Jepson
References to other publications
(i) Public Health England. Health matters: getting every adult active every day. 19 July 2016.
(ii) Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public health reports. 1985.
(iii) World Health Organisation. Global action plan on physical activity 2018-2030; more active people for a healthier world. 2018.
(iv) UK Chief Medical Officers Recommendations 2017: physical activity in pregnancy. 2017.
(v) World Health Organization. Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. 2019.
(vi) Reily JJ, Hughes A, Janssen X et al. UK physical activity guidelines: draft review and recommendations for the under 5s, October 2018 UK Expert Committee for Physical Activity.
(vii) Department of Health. Policy Research Programme summary final report form: Empower – empowering mothers to prevent obesity at weaning 060/0003. 2011.
(viii) Sport England. Active Lives children and young people; attitudes towards sports and physical activity 2019.
(ix) Mansfield L, Kay T, Meads C, et al, Sport and dance interventions for healthy young people (15–24 years) to promote subjective well-being: a systematic review, BMJ 2018.
(x) Public Health England. Muscle and bone strengthening and balance activities for general health benefits in adults and older adults. 2018.
(xi) HM Government. Childhood obesity: a plan for action, chapter 2. 2016.
(xii) Engaging adolescents in changing behaviour (EACh-B): a programme of research to improve the diets and physical activity levels of teenagers Barker M.
(xiii) Tuvey S, Steele J, Horton E, Mayo X, Liguori G, Mann S, et al. Do changes in cardiorespiratory fitness resulting from physical activity interventions impact academic performance and executive function in children and adolescents? A systematic review, meta-analysis, and metaregression.2019.
(xiv) Sport England. Active Lives Adult Survey November 17/18 report.
(xv) Howlett, N., Trivedi, D., Troop, N. A., & Chater, A. M. (2018). Are physical activity interventions for healthy inactive adults effective in promoting behavior change and maintenance, and which behavior change techniques are effective? A systematic review and meta-analysis. Translational behavioral medicine.
(xvi) Sport England. Active Lives adult survey November 17/18 report.
(xvii) Smith L, Ekelund, U, Hamer M. The Potential Yield of Non-Exercise Physical Activity Energy Expenditure in Public Health (2015) Sports Medicine.
(xviii) Pavey TG, Anokye N, Taylor AH, Trueman P, Moxham T, Fox KR, Hillsdon M, Green C, Campbell JL, Foster C, Mutrie N. The clinical effectiveness and cost-effectiveness of exercise referral schemes: a systematic review and economic evaluation. Health Technology Assessment. 2011.
(xix) Public Health England. Changing risk behaviours and promoting cognitive health in older adults; an evidence-based resource for local authorities and commissioners. 2016.
(xx) Banks, J., Batty, GD., Coughlin, K., Deepchand, K., Marmot, M., Nazroo, J., Oldfield, Z., Steel, N., Steptoe, Wood, M., A Zaninotto, P. (2019). English Longitudinal Study of Ageing: Waves 0-8, 1998-2017.
(xxi) Ukactive. Moving more, ageing well. 2017.
(xxii) National Institute for Health and Care Excellence. NICE Guideline [NG90] Physical activity and the environment.2018.
Acknowledgements
This report was written by Duncan Fortescue-Webb with Tansy Evans, Katharine Hanss and Tara Lamont of the NIHR Dissemination Centre.
Expert input was provided by a steering group consisting of:
Hannah Behrendt – Senior Advisor, Behavioural Insights Team, Cabinet Office
Michael Brannan – National Lead for Physical Activity, Public Health England
Angel Chater – Deputy Director, Institute for Sport and Physical Activity Research & Chair, Behavioural Science and Public Health Network
Allison Coles - Research, Insight and Projects Manager, British Cycling
Andy Cope – Director of Insight, Sustrans
Michael Dooley – Previous Director of Sports Medicine and Science to the British Equestrian Team & Medical Director of The Poundbury Clinic
Deborah Hardoon – Head of Evidence, What Works Wellbeing
Philip Insall – Public Contributor
Andrew Morrison – Deputy Director, Local Transport, Local and Regional Transport Analysis, Department for Transport
Vincent Paliczka – Hon. Treasurer, Chief Cultural & Leisure Officers Association & Director of Environment, Culture and Communities, Bracknell Forest Council
Sarah Ruane – Strategic Lead for Health, Sport England
Russ Jago – Professor of Paediatric Physical Activity & Public Health, University of Bristol
Rupert Suckling – Director of Public Health, Doncaster Council
James Steele – Associate Professor of Sports and Exercise Science, Southampton Solent University & Principal Investigator, ukactive
Julia Thrift – Projects & Operations Director, Town & Country Planning Association
Helen Walters – Public Health Consultant Advisor, National Institute for Health Research
Tom Yates – Professor of Physical Activity, Sedentary Behaviour and Health, University of Leicester
Produced by the University of Southampton on behalf of NIHR through the NIHR Dissemination Centre
